Abstract:
Middle East respiratory syndrome (MERS) is a rare, acute and sometimes fatal human disease affecting mostly those who live in (or travel to) the Arabian Peninsula. First identified in 2012, this disease affects the respiratory system and is fatal in 20-40% of those infected. The following article provides an introduction to this emerging infectious disease.
Main Article:
Middle East respiratory syndrome (MERS) is a rare, acute and sometimes fatal human disease affecting the airways (and sometimes other organs), resulting directly or indirectly from infection by a newly emerged coronavirus (MERS-CoV).
Discovery
MERS-CoV was first described from a fatal infection identified in a 60-year-old man from Bisha, Jeddah in the Kingdom of Saudi Arabia (KSA).1 The world was made aware of this novel finding in September 2012 via an email to a global emerging disease mailing list, ProMED. This discovery was initiated because of the vigilance of an Egyptian virologist, Dr Ali Mohammed Zaki, who was working in a laboratory attached to the Dr Soliman Fakeeh Hospital at the time. Dr Zaki worked in collaboration with Erasmus University Medical Centre (EMC) researchers from The Netherlands to whom he sent virus. Retrospectively, cases were identified as part of an outbreak in a hospital in Zarqa City, Jordan, with onset in March of 2012. Hospital outbreaks were to become the hallmark of MERS infections for the next three and a half years.
The EMC patented that first 2012 virus isolate, naming this variant of the “novel coronavirus”, EMC/2012. Herein, I refer to a “variant” as the particular dominant virus identified from a single person or animal. A more distinct and meaningful name for all the variants, MERS-CoV, was subsequently ratified but issues around patenting of that virus have remained contentious. The EMC/2012 variant was readily provided to requesting professionals following standard transfer processes and patenting did not prevent the exceptionally rapid development and publication of validated PCR-based diagnostic assays, used to this day. However, the process of patenting did slow the commercialization of essential antibody detection tools. The need to pay royalties, which raises the cost of test kits, and the extra legalities involved have not halted in-house assay development and validation, but they have hindered very valuable methods from evolving beyond the research settings.
Geographic Distribution
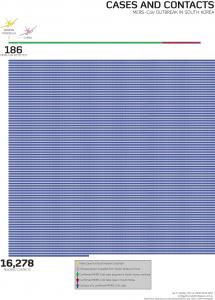
Since March 2012, 80% of more than 1,600 MERS-CoV infections have been detected in the KSA, with 25 other countries recording a case, 12 of those resulting in local case spread. The largest outbreak outside the Arabian Peninsula occurred in healthcare facilities in South Korea2. Beginning in May 2015, the outbreak comprised 186 cases and 37 deaths and was fuelled by a spectrum of circumstances that supported and maintained the spread of infection.
Zoonosis
From very early on, the dromedary camel (DC) was implicated as a possible reservoir for human infection. Bats were also implicated, largely by default since a vast array of different CoVs had already been found in them over preceding years. However, apart from a single, short, sequenced diagnostic PCR product from one sample from one bat of one species that was part of 1,003 bat samples, no MERS-CoV variants have been detected, sequenced or infectious virus isolated (grown in culture) from a bat.
MERS-CoV in camels is akin to the impact of rhinoviruses in humans: a common cold virus
MERS-CoV variants have however been detected, with significant frequency, from DC upper respiratory tract swabs and, less frequently, from rectal swabs and faeces. In one study, virus RNA was found in camel milk and in another, from the air of a barn housing an infected DC. MERS-CoV spreads rapidly throughout a herd, with each camel yielding detectable viral RNA for about a week.10 There are also signs that camels can be reinfected by the virus, which manifests in them as no more than a common cold; a running nose is the most common symptom, along with a raised temperature. In this sense, MERS-CoV in camels is akin to the impact of rhinoviruses in humans: a common cold virus. It can be assumed that infectious camel nasal secretions, which may harbour high viral loads, are the source of viral spread among camels in herds. Many studies have also found signs of MERS-CoV antibody in camel samples, so far dating back 30 years.
Human Transmission
MERS severe enough to warrant admission to hospital occurs rarely, yet most frequently among older males who already have an underlying disease, notably diabetes, heart disease or lung disease. MERS-CoV is an opportunistic virus, a fact also supported by the high rate of hospital acquired cases, clusters and outbreaks. Transmission of virus in medical care facilities is more often responsible for human cases than the less frequent direct contact with camels. Outside a health care setting, and despite the many opportunities afforded by some of the world’s largest mass gatherings and human migrations held in the KSA, MERS-CoV has been a poorly transmitting virus in humans. We can speculate that we only see MERS, the disease, because of the already ill health of a portion of the community, especially in the KSA. Much more work needs to be done to understand relatively rare transmission events which are mostly caused by a range of underpinning lapses in, and poor understanding of, infection control and prevention (ICP). The proportion of primary cases is between 7% and 38% of all MERS cases in the KSA, depending on the source of publicly available data (the WHO or KSA Ministry of Health, respectively). Health care facility outbreaks are only controlled after improving ICP processes. How the virus spreads from human to human is unclear; it may require extended and close contact, larger wet droplets, lighter floating droplet nuclei, high risk mechanical procedures, fomites or, most likely, a mix of all these things. MERS-CoV is stable on surfaces and in fluids at different temperatures for a range of time periods.
The majority of contacts of confirmed MERS cases do not develop disease, but further serosurveys would better define whether subclinical transmission is occurring and its role, if any, in chains of transmission (perhaps prospective high-frequency sampling of willing contacts of confirmed cases). Mild and asymptomatic infections are reported, so we already know that MERS-CoV gives rise to the full spectrum of clinical outcomes, but we do not know if these subclinical cases shed infectious virus in quantities that result in the infection of others. Relying on relatively insensitive virus culture – at least insensitive compared to PCR-based technologies – may not be reliably informing us of community virus travel.
Epidemiology
MERS-CoV has been shown to be an antigenically stable virus thus far, with nearly all variants comprising a single serotype.3 There are multiple reports of sequence mutation, deletion and recombination, but to date these have had no clinically-relevant implications for disease nor on transmission.4 6 Empirical investigations of the impact of genetic changes are ongoing. Full genome sequencing of MERS-CoV variants define the existence of two genetic groups or clades, A and B. Clade A contains just the earliest viruses from Bisha and Zarqa City; why these have not continued to circulate, or be detected, is unknown. Clade B is a container for all other human and the majority of DC variants. Clade B virus genomes, whether from human or camel, share over 99% nucleotide identity; they are very similar. Studies of camels sent to abattoirs in Egypt and Nigeria have found variants comprising a third, non-Clade A, non-Clade B lineage of MERS-CoV variants which are more divergent than those found in the Arabian Peninsula.9 This new lineage hints at ancestral MERS-CoV viruses residing in the camels of African nations, but little is known of their nature yet.
The obvious question arises of why countries with DCs that show signs of prior infection or harbour divergent MERS-CoV variants are not also among the 26 countries to report human cases of MERS. An absence of reporting may relate to differences in farming practices (camel densities, handling, milking and butchering), differences in overall human population health (fewer or different comorbidities) or most simply, an absence of strategic studies seeking MERS-CoV infections. It is known that camels are imported to the Arabian Peninsula from African countries known to have MERS-CoV infected camels and this is a possible source for the establishment of MERS-CoV, which is now enzootic throughout the Arabian Peninsula.8 A vaccine to address this infection in DCs is under development but has yet to completely stop symptomatic shedding from infected animals.7
Considerable knowledge gaps remain in our understanding of the spread of MERS-CoV
Considerable knowledge gaps remain in our understanding of the spread of MERS-CoV. For now, MERS-CoV is known to be a poorly transmitting virus in humans, but a serious health threat to a small section of some communities. In camels, MERS-CoV is a widely-spread, milder annoyance; they have no equivalent to MERS disease. MERS-CoV is spread among humans because of human behaviours, mostly in health care settings that display an inadequate understanding of the roles, methods and importance of ICP. The virus has its greatest impact among older males with diabetes and heart disease. Were these training, communication, behavioural and societal issues to be addressed, we would see very few cases of MERS anywhere in the world.
References:
- Mackay I.M., K.E. Arden (2015, December). MERS coronavirus: diagnostics, epidemiology and transmission. Virology Journal 12(1):222. Retrieved from: http://www.ncbi.nlm.nih.gov/pubmed/26695637
- Death toll of MERS reaches 37 in S. Korea. (2015, October 25). [Article on Yonhap News Agency]. Retrieved from: http://english.yonhapnews.co.kr/national/2015/10/25/99/0302000000AEN20151025002300320F.html
- Muth, D. et al. (2015, September). Infectious Middle East Respiratory Syndrome Coronavirus Excretion and Serotype Variability Based on Live Virus Isolates from Patients in Saudi Arabia. Journal of Clinical Microbiology, 53(9):2951-5. Retrieved from: http://www.ncbi.nlm.nih.gov/pubmed/26157150
- Dudas, G. and A. Rambaut (2015, December). MERS-CoV recombination: implications about the reservoir and potential for adaptation. [Article on bioRxiv]. Retrieved from: http://biorxiv.org/content/early/2015/06/12/020834
- Wang, Y et al. (2015, September). Origin and Possible Genetic Recombination of the Middle East Respiratory Syndrome Coronavirus from the First Imported Case in China: Phylogenetics and Coalescence Analysis. mBio vol. 6 no. 5. Retrieved from: http://mbio.asm.org/content/6/5/e01280-15.full
- Sabir, Jamal, T. Lam, M. Ahmed, L. Li, et al. (2015, December). Co-circulation of three camel coronavirus species and recombination of MERS-CoVs in Saudi Arabia. [Article on Science]. Retrieved from: http://www.sciencemag.org/content/early/2015/12/16/science.aac8608.long
- Haagmans, BL et al. (2015, December). An orthopoxvirus-based vaccine reduces virus excretion after MERS-CoV infection in dromedary camels. [Article on Science]. Retrieved from: http://www.ncbi.nlm.nih.gov/pubmed/26678878
- Hemida, MG. et al. (2015, August 10). Dromedary Camels and the Transmission of Middle East Respiratory Syndrome Coronavirus (MERS-CoV). [Transboundary and Emerging Diseases. doi: 10.1111/tbed.12401]. Retrieved from: http://www.ncbi.nlm.nih.gov/pubmed/26256102
- Chu D, Oladipo J, Perera R, Kuranga S, Chan S, Poon L, Peiris M. (2015, December 10). Middle East respiratory syndrome coronavirus (MERS-CoV) in dromedary camels in Nigeria, 2015. Eurosurveillance, Vol. 20, Issue 49. Retrieved from: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=21327
- Wernery U, Corman VM, Wong EYM, Tsang AKL, Muth D, Lau SKP, et al. (2015, June). Acute Middle East respiratory syndrome coronavirus infection in livestock dromedaries, Dubai, 2014. Emerging Infectious Diseases, vol. 21, no.6. Retrieved from: http://wwwnc.cdc.gov/eid/article/21/6/15-0038_article













[…] An introduction to the Middle East respiratory syndrome (MERS) a rare, acute and sometimes fatal human disease. […]