Abstract:
Bacteraemia is indicated by the presence of pathogens in blood. As this is systemic, bacteraemia can become fatal very quickly. In the United Kingdom, the institution of surveillance programs has decreased the incidence of both methicillin-resistant Staphylococcus aureus-borne bacteraemia and general Clostridium difficile infections. As a result, patient mortality following bacteraemia is reduced, but the incidence of infections has shifted from the clinic to the community. At the Knowlex National 2016 Infection Prevention and Control Conference in Manchester, England, Russell Hope discussed the effects of the surveillance programs.
Main Article:
The surveillance of infections by methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile have been closely monitored since 2001 in the United Kingdom, as they were identified as key infections with the capacity to cause widespread fatalities across the UK and beyond. By seeing not just the number of infections, but also their causes and other conditions related to the illness, public health agencies can design programs to reduce these infections.
Since the early 1990’s, there has been a steady increase in cases of bacteraemia (presence of bacteria in the blood) caused by MRSA. MRSA-borne bacteraemia cases reached almost 6,000 cases annually in the UK, and slowly increased to nearly 9,000 cases by 2002.1,2 It was at this point that surveillance first began, and there has been a steady decrease in MRSA-borne bacteraemia since its introduction. In 2003, a goal to reduce this incidence by 50% in the UK was set, which was aided by instituting improved, more comprehensive surveillance protocols in 2005, 2010, 2011 and 2013.1,3 Since then, the number of methicillin-resistant S. aureus infections have decreased significantly to only 820 cases in 2015.1 However, for disputed reasons, the occurrence of methicillin-sensitive Staphylococcus aureus-borne bacteraemia has changed minimally in the same time period (Figure 1).1
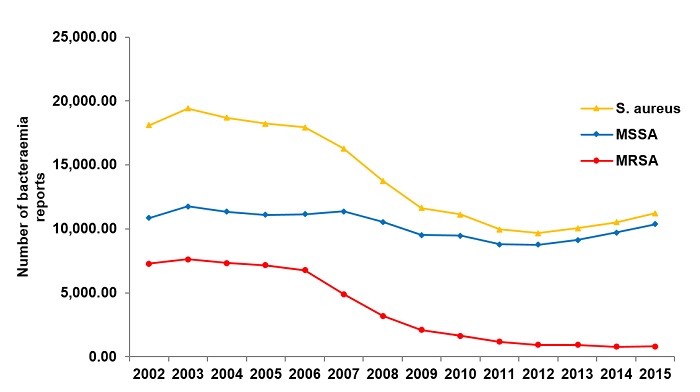
Figure 1- Bacteraemia rates in the United Kingdom from 2002 to 2015.
During this period, the development of MRSA has changed from a predominantly hospital acquired infection to a more community associated infection. This was determined by tracking the development of MRSA within two days of hospital admission and its development seven days after hospital admission, which typically coincides with discharge from the hospital.3 This may be indicative of better practices in surveillance and cleaning in the hospitals. The incidence of catheter and main line infections significantly decreased in this period, whereas skin and soft tissue infections increased proportionally.4
In 2013, a post-infection review from Public Health England began to further involve the community in MRSA control. The public Trust aimed to identify ways in which community-acquired MRSA bacteraemia could have been avoided.
Molecular diagnostics of MRSA-bacteraemia show that previously predominant strains are less infective in recent years, but this is matched by an increase in the variety of different MRSA strains spread across the UK.
Additionally, by monitoring mortality rates in bacteraemia patients, a significant decrease in the number of deaths caused by MRSA is seen (Figure 2).1 Based on other data, not only is the incidence of MRSA-borne bacteraemia decreasing, but in cases where patients are being infected, patient survival is much greater than in the past.
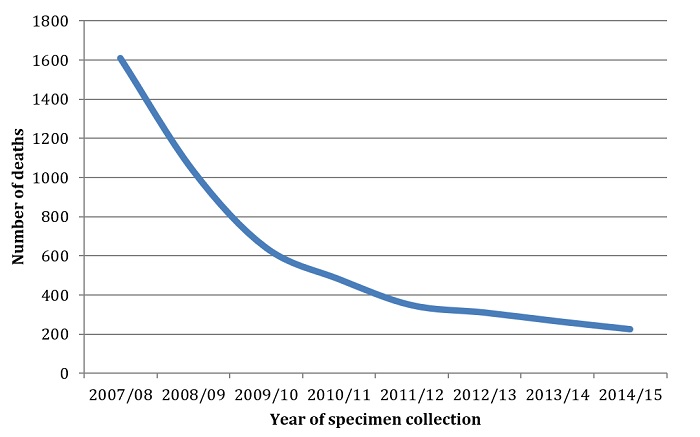
Figure 2: Number of Deaths Within 30 days of Specimen Collection by Infection
Clostridium difficile Monitoring
The effects of surveillance are not unique to MRSA. Around the same time, the monitoring of C. difficile cases began, and similar trends can be seen (Figure 3).5 With the peak of infections and subsequent institution of monitoring programs in 2007, there was a marked decrease and continuing downward trend in the number of C. difficile infections.5 Following these infections, with greater surveillance, C. difficile infections also became less fatal and more community-associated, as opposed to hospital acquired.
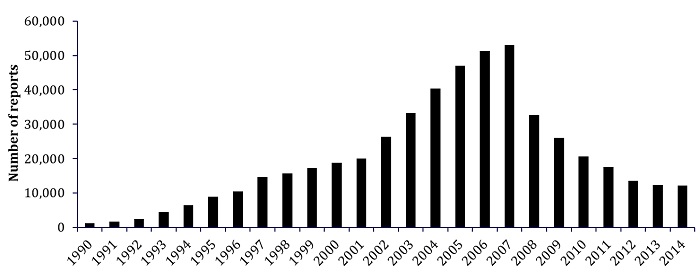 Figure 3: Number of C. difficile infections in England from 1990 to 2014.
Figure 3: Number of C. difficile infections in England from 1990 to 2014.
Conclusions:
The long term benefits of increased surveillance are being realized today. Due to the UK’s efforts, the incidence and severity of MRSA and C. difficile infections have decreased dramatically. From the early 1990’s to the mid 2000’s, there was a steady incidence and mortality rate associated with C. difficile and MRSA-borne bacteraemia. With the surveillance programs in place, the reduction in catheter and main line associated infections decreased. This shifted a great proportion of infections to the community, but absolute infection rates are still down. With this information, global surveillance programs have the potential to tackle bacteraemia rates worldwide.
Watch the presentation here: https://youtu.be/qfBtJBR-5Kw
References:
- MRSA Action UK (2016). MRSA and Clostridium difficile Accessed September 28, 2016. http://mrsaactionuk.net/monthlystatistics.html
- Johnson, A. P., Pearson, A., & Duckworth, G. (2005). Surveillance and epidemiology of MRSA bacteraemia in the UK. Journal of Antimicrobial Chemotherapy, 56(3), 455-462.
- Johnson, A. P., Davies, J., Guy, R., Abernethy, J., Sheridan, E., Pearson, A., & Duckworth, G. (2012). Mandatory surveillance of methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia in England: the first 10 years.Journal of antimicrobial chemotherapy, dkr561.
- Daum, R. S. (2007). Skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. New England Journal of Medicine, 357(4), 380-390.
- Public Health England (2014) Clostridium difficile infection: annual data. Accessed September 28, 2016. https://www.gov.uk/government/statistics/clostridium-difficile-infection-annual-data











