Abstract
Some of the most communicable infectious diseases present with fever when they are most contagious.
Diseases like flu, norovirus, Ebola, measles and tuberculosis all pose a threat to travellers, hospital patients, and ordinary citizens when the disease carrier boards an airplane, enters a hospital ward or simply handles food in a busy restaurant. For those people who do not heed the advice of the Centers for Disease Control of “stay home from work, school, and errands when you are sick,” we need a system of early detection in place to help prevent the spread of disease.
An accurate, self-service screening system can also be an effective tool for public health departments, enabling them to obtain an actual assay of the specific disease for which a patient may require immediate quarantine or treatment, allowing for the best possible health outcome. Such measures greatly reduce both the spread and the evolution of many contagious diseases.
Long term public health could be positively impacted with the identification, tracking and monitoring of illnesses. The collection of data will inform the need for preventative measures, including the development and promotion of vaccines, the development of improved personal hygiene and cleaning specifications and specific public health campaigns to identify the symptoms, signs and dangers of a particular disease.
Main Article
Fever as an Indicator of Infection
A fever occurs when an infection is so extensive that the hypothalamus, the part of the brain that detects body temperature, is deceived into thinking that the body temperature is cooler than it is. The hypothalamus responds by raising the body temperature, thus inducing fever (Center for Disease Control & Prevention, 2015).
Although elevated body temperature can be caused by many factors, including severe sunburn, certain inflammatory conditions and certain immunizations, fever is also a symptom in many infectious diseases. At the point when the illness causes fever, the number of viruses in the body is astronomical. Viruses in this stage can grow in population from thousands to millions in hours. In response, the body releases hormones to raise temperatures to attenuate its spread. Meanwhile, the “live contagion” can opportunistically evolve and migrate to organs (such as the lungs) that can further spread the virus to other people through airborne, fomite or casual contact (Center for Disease Control & Prevention, 2016b).
fever is a primary indicator of a live infection
The presence of fever is a primary indicator of a live infection. If rapid contagion screenings became commonplace among employees and at airports and other ports of entry, then people with contagious disease would potentially come under scrutiny and receive medical attention before they are able spread disease (World Health Organization, 2017). This is not only good for the infected person and the population, but is also reduces the spread of mutations and potentially more dangerous pathogens.
Rapid Contagion Screenings in Food Service
In August 2015, hundreds of customers of a Chipotle restaurant in Simi Valley, California fell ill with what was later identified as Norovirus (Flynn, 2015). Norovirus can cause a highly contagious form of viral gastroenteritis. Common symptoms include diarrhea, vomiting, stomach pain, fever, headache and body aches. (CDC, 2016a). The virus can be spread through contact with an infected person or contaminated surface, or through contaminated food or water. In the case of Chipotle’s outbreak, the company has identified the original source of the disease as sick employees (Whitten, 2016). The outbreak caused the affected restaurant to close for a period of time, causing both a loss of business and customer confidence. In response to the crisis, the restaurant chain has introduced measures to avoid a similar situation in the future.
While measures such as improved sanitation practices and paid sick leave are positive approaches to prevention, another tool is a method of rapid “contagion” screening of employees before granting access to food preparation or public areas of the restaurant. A screening zone that reports the presence of a fever, together with policies that support the appropriate action to be taken by managerial staff, could make the food prep environment more sterile (Center for Disease Control and Prevention, 2015). Implementing such a system will also give wary customers some assurance that the restaurant takes its obligation toward their health and safety seriously.
Rapid Contagion Screening in Hospitals
A study published in the JAMA Pediatrics revealed that, despite 95% of respondents to a survey holding the belief that working while sick put patients at risk, 83% of those same healthcare workers did, in fact, report to work when suffering a variety of symptoms, including diarrhea, fever and acute onset of respiratory symptoms (Szymczak et al, 2015). Healthcare workers are 1.5 times more likely to develop infectious illnesses than non-health care workers (Wallace, 2016). Their increased risk of obtaining respiratory and/or gastrointestinal illnesses stems from their increased exposure to bacteria and viruses in the hospital setting.
A variety of reasons are given by healthcare workers for working while sick, including sociocultural factors, such as feelings of obligation to colleagues and to patients, fear of ostracism by colleagues, concern about continuity of care, unsupportive leadership, and a perception that replacement staff is not readily available (Szymczak et al, 2015).
Another risk to patients in hospitals and nursing homes are visitors to the facility who may be sick. Most visitor policies require self-screening, imploring family members and friends to not visit if they have symptoms of, or have been exposed to, a contagious disease. Many policies indicate that visitors will be screened for infectious diseases (Center for Disease Control and Prevention, 2015). However, these screenings usually entail nothing more than a visual inspection and a written questionnaire. Unfortunately, sick people don’t always look sick, and people are not always honest in self-assessment.
Patients who are already vulnerable should not be put at further risk by their physician, nurse or visitors. Consistent, direct education as to the risks of exposing patients to contagions is crucial in changing this culture. In addition to education, the implementation of mandatory preventative fever screenings would take the decision to work or visit out of the hands of the individual. Contagions that are discovered early on by an elevation in temperature can then be appropriately managed and can potentially reduce the impact and the spread of that illness.
Rapid Contagion Screening in Airports
As seen with the Ebola outbreak of 2014, global threats can occur suddenly and without warning. Ebola was especially a problem at airports with infected patients unknowingly spreading the infection in its early stages. Airports in five U.S. cities responded with additional levels of screening for people travelling from Guinea, Sierra Leone and Liberia, including 1-2 temperature readings (Center for Disease Control and Prevention, 2014). This global threat had a major impact on international travel for many months.
According to the World Health Organization (WHO), the risk of contracting an infection on the flight itself is not of major concern. Airplane ventilation systems are comparable to those used in hospital operating rooms and intensive care units (World Health Organization, 2017). The risk of travel comes in the transport of contagious diseases across geographic regions, be it countries or states. For that reason, the WHO, CDC and airlines all advise against traveling while experiencing symptoms of having a contagious disease. Airlines may deny boarding to passengers who appear to be infected with a communicable disease (World Health Organization, 2017). Despite this authority, there is no doubt that sick people are permitted on flights every day.
In response to the specific threat of Ebola in 2014, thermal scanners were introduced in airports in many countries, including the United States, Canada and the United Kingdom. This was instituted as a primary entrance screening tool for fevers, a symptom of Ebola (Bogoch, 2015). More widespread implementation of primary fever screening at airports would ensure that passengers presenting with fever receive further screening to ensure that those with communicable diseases are not permitted to fly.
High Tech Solution
A hands-free screening device, such as a computer-aided thermal sensor (WelloStation, Wello Inc.) that reads body temperatures, could screen many more people in much less time than traditional thermometers, allowing airports to quickly check people from more countries, not just those on the flagged list. Relatively inexpensive to maintain, this high-tech device could potentially save incredible amounts of money that is currently being spent on less effective measures. In addition, its use is touch-free to prevent the spread of any bacteria. Scanners could be implemented in food service venues, schools, hospitals and other workplaces and public spaces to contribute to the early detection and treatment of infectious diseases.
School systems in Dallas that were under watch for Ebola utilized the WelloStation system. During the Ebola crisis, the WelloStation took and recorded the temperature of each person entering the school; if a fever was present, that person was flagged and sent confidentially to the administrator. If it was a child, a parent was automatically notified (Wello, 2016). The WelloStation has effectively been used in dental offices, jails, hospitals and factories.
Data analysis would take on a whole new dimension
Having an early detection tool in place could mean an enormous shift in the way we are able to detect and monitor the spread of illnesses. Data analysis would take on a whole new dimension, as diseases could potentially be tracked and monitored in a much more effective manner. Surveillance of disease trends could open up new information to consider in the field of practical infection prevention. New knowledge gained from this data could be applied toward preventative measures. The results of disease prevention could be seen globally, potentially saving lives and untold amounts of money spent on disease treatment.
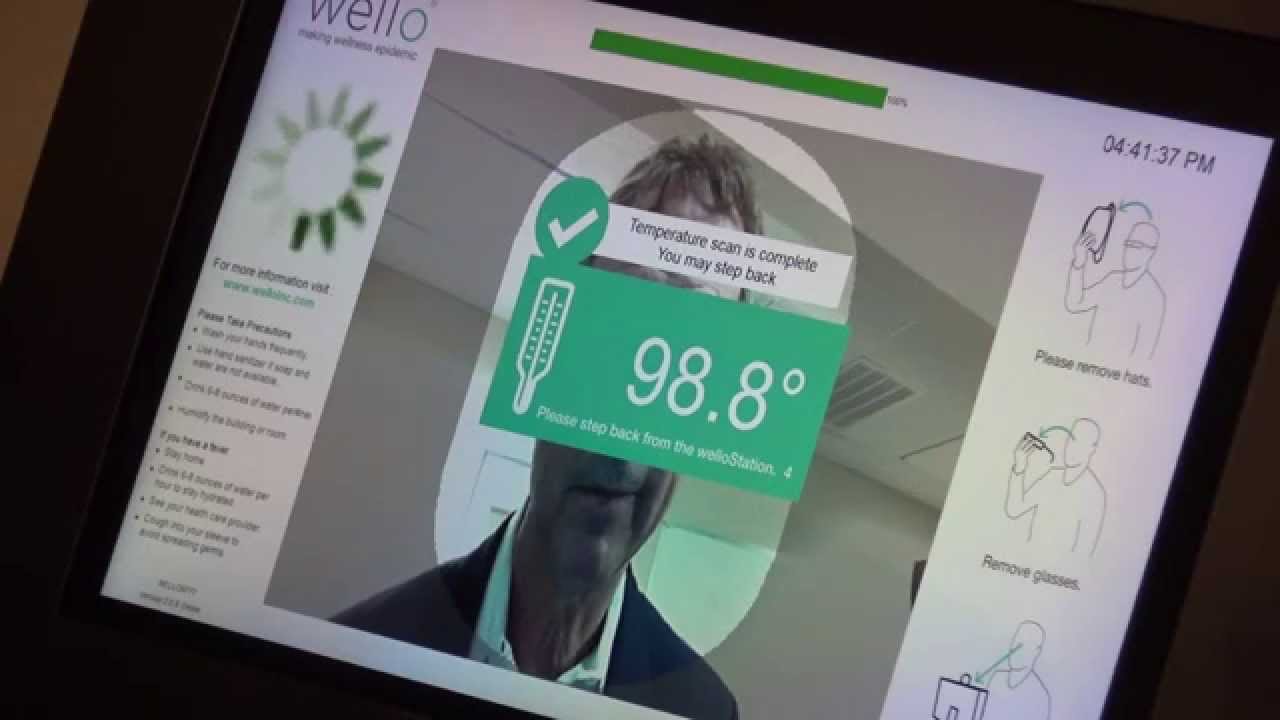 Figure 1: WelloStation in use providing the user and facility accurate and rapid temperature reading.
Figure 1: WelloStation in use providing the user and facility accurate and rapid temperature reading.
References
- Bogoch, I. I., Creatore, M. I., Cetron, M. S., Brownstein, J. S., Pesik, N., Miniota, J., . . . Khan, K. (2015). Assessment of the potential for international dissemination of Ebola virus via commercial air travel during the 2014 west African outbreak.The Lancet, 385(9962), 29-35.
- Center for Disease Control & Prevention. (2016a). Multistate Outbreaks of Shiga toxin-producing Escherichia coli O26 Infections Linked to Chipotle Mexican Grill Restaurants (Final Update). Retrieved from: https://www.cdc.gov/ecoli/2015/o26-11-15/index.html
- Center for Disease Control & Prevention (2016b) Norovirus (2016, August 30). Retrieved February 19, 2017, from https://www.cdc.gov/norovirus/index.html
- Center for Disease Control & Prevention (2015).Stopping the Spread of Germs at Home, Work & School. (2015, August 19). Retrieved February 19, 2017, from https://www.cdc.gov/flu/protect/stopgerms.htm
- Center for Disease Control & Prevention. (2014). Enhanced Ebola Screening to Start at Five U.S. Airports and New Tracking Program for all People Entering U.S. from Ebola-affected Countries. Retrieved from: https://www.cdc.gov/media/releases/2014/p1008-ebola-screening.html
- Flynn, D. (2015). Chipotle’s First Norovirus Outbreak in California was Larger Than Boston College’s. Food Safety News. Retrieved February 19, 2017, from http://www.foodsafetynews.com/2015/12/chipotles-first-norovirus-outbreak-in-california-was-larger-than-boston-colleges/#.WKnsAPkrLIV
- Szymczak JE, Smathers S, Hoegg C, Klieger S, Coffin SE, Sammons JS. Reasons Why Physicians and Advanced Practice Clinicians Work While Sick: A Mixed-Methods Analysis. JAMA Pediatr.2015;169(9):815-821.
- S. Food and Drug Administration. (2016). FDA Investigates Multistate Outbreak of E. coli O26 Infections Linked to Chipotle Mexican Grill Restaurants. Food Drug Administration. Retrieved from: http://www.fda.gov/Food/RecallsOutbreaksEmergencies/Outbreaks/ucm470410.htm
- Valuentum Team. (2016). Chipotle Not Showing Signs of Recovery. Retrieved from: http://seekingalpha.com/article/4027041-chipotle-showing-signs-recovery
- Wallace, N. (2016). Hospital Infections: The Impact on Healthcare Worker Absenteeism. InfectionControl.tips. 8, 1-4. Retrieved from: https://infectioncontrol.tips/2016/08/24/hai-worker-absenteeism-931/
- Wello (2016). Channel 11 Newscast. Youtube. Retrieved from: http://www.welloinc.com
- Whitten, S., & Wang, C. (2016). Chipotle safety meeting addresses multiple illness culprits. CNBC. Retrieved February 19, 2017, from http://www.cnbc.com/2016/02/08/chipotle-blames-norovirus-outbreaks-on-sick-employees.html
- World Health Organization (2017) Transmission of communicable diseases on aircraft. World Health Organization Retrieved February 20, 2017, from http://www.who.int/ith/mode_of_travel/tcd_aircraft/en/