Peer Reviewed
Disclosures: Dr. Tamás Haidegger is a co-founder and CEO of HandInScan. The remaining authors of this report and InfectionControl.tips declare no conflict of interest with the following research.
Editor Note: Correct Order of Authors is as follows: Andrew Duong, Tamás Haidegger, Dr. Jason Davies, Dr. Michael Ackerman
Abstract
Hands are an important link in the chain of infection. Unclean hands are often the culprit for the spread of numerous infectious diseases, but the risk can be mitigated through an appropriate hand hygiene regimen. In this study, participant attitudes towards hand hygiene and the efficacy of hand disinfection with an alcohol-based hand rub (ABHR) were tested using a questionnaire and a computer-aided Semmelweis Hand Hygiene Scanner. Most subjects reported that their use was dependent on the availability of disinfectant dispensers. The majority of subjects did not sufficiently cover their hands with the disinfectant; most often missing their fingertips and dorsal surface. The use of the Semmelweis Scanner provided real time results for the subjects, who were overwhelmingly open to improving their own hand hygiene technique following evaluation.
Introduction
The spread of infectious diseases is often associated with nosocomial or hospital-acquired infections. There are many reasons for this predominance, but studies have consistently identified the hands of patients and healthcare workers as the most common vector (1–3). Public health agencies from around the world have sought to address these preventable infections with a variety of tools. Hand washing programs have been reported to be particularly effective in improving patient outcomes. Programs to train the public in proper hand washing techniques and increasing hand washing frequency have improved hand washing compliance, and thus decreased hospital-acquired infection rates (4,5).
When hand washing facilities are not available, one alternative is to provide hand sanitizing solutions for use. These include alcohol-based hand rubs (ABHR), which can easily disinfect hands, and only require a small personal portion or a wall-mounted dispenser, instead of a sink with running water and hand drying facilities (6). In a 2014 evaluation of hand sanitizers, it was found that, although the hand sanitizers were effective in reducing the bacteria present on the subjects’ hands, the greatest variable was in the quality of the hand rub technique itself (5,6). In addition, some subjects suggested that the use of hand sanitizers is preferable over traditional hand washing. Benefits include ease of use, less drying/irritation to hands, feeling of hands following disinfection, and the availability of cleaning facilities (7,8).
In this study, we will evaluate a diagnostic scanner that analyzes a subject’s hand to detect coverage by an ABHR. This tool can be employed as a training tool to teach users about appropriate hand rubbing technique, and potentially reduce hand-borne pathogens as a source of disease.
Methods
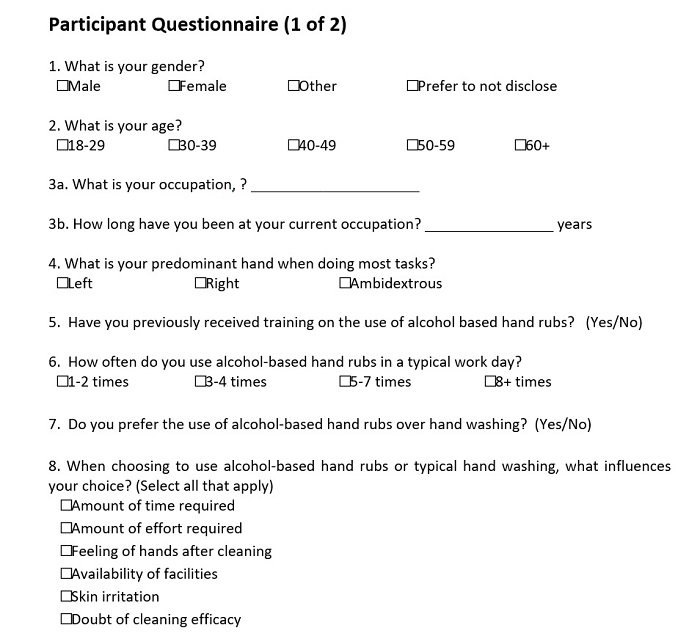
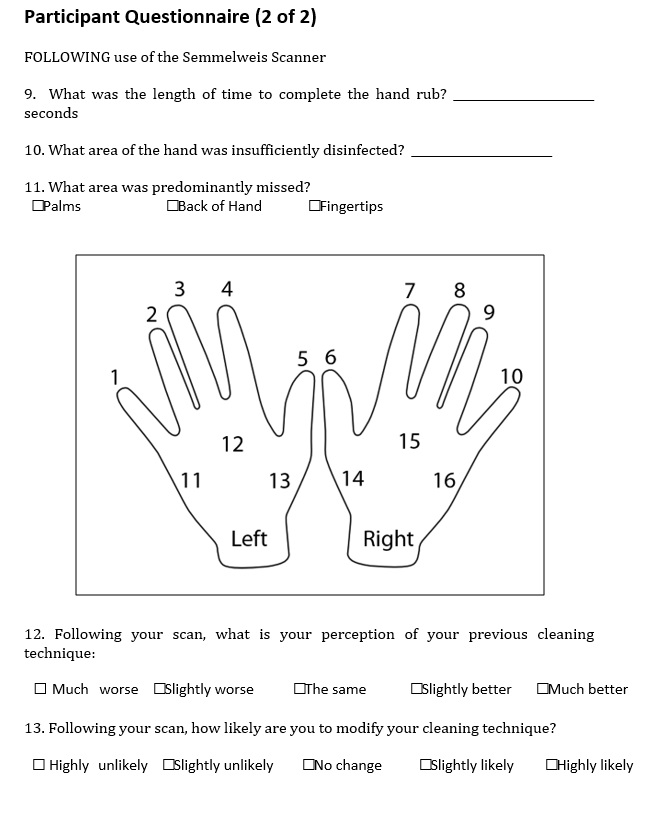
Subjects were recruited by convenience sampling from the University of Buffalo and Niagara University (Buffalo, NY), on a voluntary basis. They were asked to fill out a short questionnaire that was adapted from Harnoss et al. (2014) (Appendix 1). Following the first half of the questionnaire, the subjects were requested to use the ABHR, which included a UV fluorescent dye (Visirub Training Hand Rub, Hartmann Gruppe). The length of decontamination was timed and recorded by a research assistant. Following this, the subjects placed their hands into the Semmelweis Scanner (HandInScan Zrt, Budapest, Hungary), which takes an image of the subject’s hand, and digitally evaluates it. (9). Following this, subjects filled out the remainder of the questionnaire.
Results
One hundred and thirteen subjects were recruited from both sites, where 60.2% were female. The majority of respondents were between the age of 18 and 29 years (51.8%), and were students (46.4%) or nurses (21.1%). Nurses were in practice for an average of 20.3 years. All students were post-secondary students.
Most respondents (60.5%) had not received any training in the use of ABHR. Respondents who did receive training in the appropriate use of ABHR typically used them 5–7 times throughout the day, whereas those without training were likely to use them 1–2 times a day. Students were more likely not to receive any training in the use of the ABHR. Most respondents (69.2%) prefer hand washing over the use of ABHR when facilities are available. When choosing to use an ABHR, the strongest influencing factors were the availability of facilities (24.5%), the feeling of their hands after use (21.7%), and the amount of time required (19.7%). Interestingly, 10.7% of respondents stated that ABHR were used less due to distrust of cleaning effectiveness.
During the evaluation of hand rub efficacy, most subjects cleaned their hands for 19.21 ± 7.85 seconds (mean ± standard deviation), ranged from 7.20 seconds to 60.00 seconds in duration for the entire cohort. Only eight subjects (six students and two nurses) were capable of complete coverage of their hands using the ABHR. These subjects used the hand rub for an average of 26.95 seconds; of these, both nurses and one of the students had previous training regarding the appropriate use of the hand rub.
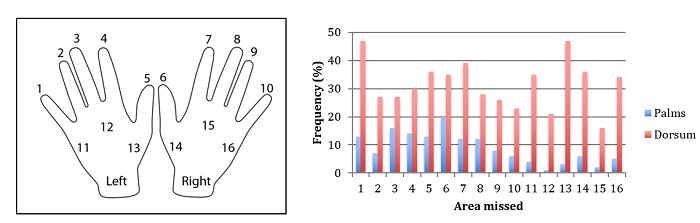
Most subjects were able to ensure complete coverage of their palms, (Figure 1). Interestingly, the dominant hand did not have an effect on the coverage of either hand, but the majority of subjects (85.8%) were right hand dominant. For both hands, the finger tips were most often missed, and this was especially exacerbated on the dorsal side (back of the hand). This was especially prevalent at the base of the thumbs, dorsally (Figure 1, areas 13 and 14). On average, subjects did not spread the ABHR to 6.27/32 different areas of their hands, as determined by the Semmelweiss scanner (Figure 1). Overall, 23.9% of subjects missed 10 areas or more of their hands.
Figure 1: Areas not covered by the alcoholic hand rub. Legend for areas is indicated.
Following the scan, subjects were asked two additional questions on their perception of their own efficacy results. The largest proportion of respondents stated that the results were slightly worse or much worse than expected, 27.9% and 23.01%, respectively, and 26.0% stated that their results were as expected. Only 18.3% and 4.8% of respondents said that they performed slightly better or much better than expected, respectively. Following the scan, most subjects stated that they were highly likely (56.6%) or likely (26.3%) to change their method of hand disinfection. This result was more striking when subjects performed worse than they expected. Of these, 98.1% of subjects stated that they were likely or highly likely to change their cleaning technique. Subjects who stated they performed better than expected only reported that they were likely or highly likely to change their cleaning techniques in 71.4% of cases.
Discussion
In this study, it was found that the majority of subjects showed insufficient hand disinfection technique when using ABHR, as demonstrated by the Semmelweis Scanner. Of the 113 subjects, comprising mostly of nurses and students, only eight demonstrated full coverage of the ABHR, as measured by the digital evaluation of the Semmelweis Scanner. The average length of time for the hand rub was 19.21 seconds, whereas the average length of hand rub use for fully covered hands was 26.95 seconds. The use of the hand scanner indicated that its use triggered a change in technique, regardless of the subjects’ performance in hand disinfection.
The majority of respondents were nurses or students. This may be indicative of the recruiting centers utilized for this study. However, both cohorts provided a unique opportunity for analysis, as multiple studies have indicated that hand hygiene compliance and competence have much room for improvement (2,10–12). In the study of students, it was found that most students have received no training in hand disinfection. In the study of nurses, most nurses were found to have received training for hand hygiene, but workload, among other factors, reduced their compliance with the techniques they learned. Regardless, additional teaching interventions have been shown to have a large impact in the improvement of compliance (10,13). Nurses spent an average of 19.05 ± 6.73 seconds (n= 24) to disinfect their hands, whereas students spent an average of 21.49 (SD=9.05, N=51) seconds disinfecting their hands. The use of ABHR is recommended for 30 seconds, but technique also plays a role. Both cohorts performed as well as the majority of other subjects, missing an average of 7.17 and 6.33 areas on their hands for nurses and students, respectively. From these results, training did not have an impact on their hand disinfection competence.
Similar to previous findings, the availability of facilities to clean hands and time constraints were two predominant factors in the decision to use an AHBR (14). Interestingly, the feeling of the subjects’ hands after use of these rubs was also a notable consideration for respondents. This suggests that, in addition to health and infection-based concerns, purchasers should also focus on the tactile feeling of the disinfectant. Individual concerns with the hand rub (feeling during use compared to feeling afterwards) were not captured in this study. The questionnaire also revealed that a large portion of subjects still have doubt about the effectiveness of ABHR in reducing the spread of disease. These subjects were less likely to opt to use a hand disinfectant over hand washing, but did not perform any worse than subjects who did not doubt the efficacy of these disinfectants. The efficacy of ABHR is well documented, and more effort towards education on its efficacy in reducing disease should be implemented.
The introduction of health education campaigns has been fairly successful in improving hand hygiene compliance in hospitals around the world. However, the quality of the studies that monitored the changes in attitudes and health have not been thorough in general, and are of relatively low study quality (15). The anecdotal improvements in hygiene following the campaigns should be developed further to allow for more rigorous testing of their effectiveness. Regardless, a few themes have emerged from these studies: in some, there were no significant changes to the amount of hand washing when these programs were instituted. Citing lack of time, constant workloads, and the lack of hand washing facilities, the authors suggest that improvements should be made in other areas instead. Hygiene education programs have been effective in increasing the use of hand disinfection stations. Possibly due to their relative ease of use, limited time investment, and ease of installation of facilities, there have been positive annual increases in hand disinfectant use in most studies (1–3,16).
Improvement of educational programs aimed towards hand hygiene should continue to improve compliance and result in the reduction of disease transmission. One large aspect of compliance however is the appropriate use of the ABHR. In this study, only 7.07% of subjects were able to successfully cover their hands with the disinfectant. The most frequently missed areas of the hands were the fingers, and the majority of the dorsal side of the hands, as has been seen in other studies as well (17). Employment of a teaching tool, such as the Semmelweis Hand Hygiene System (HandInScan Zrt.) employed in this study can provide direct, real time evaluation of a person’s hand disinfectant use. Over half (50.97%) of the respondents performed worse than they expected, suggesting poor compliance when using the disinfectant. One large benefit of this scan is that following use of the scanner, 82.8% of subjects stated that they would modify their technique for disinfection. It has been shown that additional training, followed by immediate evaluation of a technique, greatly improves hand disinfection by identifying improper hand disinfection practices (9). Automation and electronic recording from this scanner also allows infection control practitioners to regularly evaluate compliance, and to customize additional training as needed.
Conclusion
Hand hygiene efforts are still not perfect. Our studies revealed that 92.9% of subjects did not sufficiently cover their hands with the ABHR; most often missing the finger tips and dorsal sides. The use of the Semmelweis Hand Hygiene System to detect disinfectant coverage on hands provided a real time evaluation of the subjects’ disinfection method. Regardless of their testing outcome, subjects were predominantly open to improving their hand disinfection technique. This suggests that incorporation of an evaluation step following hand disinfection training could greatly improve hand hygiene performance.
Bibliography
- Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet. 2000;356(9238):1307–12.
- Pittet D. Hand Hygiene among Physicians: Performance, Beliefs, and Perceptions. Ann Intern Med [Internet]. 2004 Jul 6 [cited 2016 Jan 6];141(1):1. Available from: http://annals.org/article.aspx?articleid=717563
- Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73(4):305–15.
- Tan J, Amil K, Olivo J. Assessing Healthcare Associated Infections and Hand Hygiene Perceptions amongst Healthcare Professionals. Int J Caring Sci . 2015;1:108–14.
- Babeluk R, Jutz S, Mertlitz S, Matiasek J, Klaus C, Aiello A, et al. Hand Hygiene – Evaluation of Three Disinfectant Hand Sanitizers in a Community Setting. Nishiura H, editor. PLoS One. 2014 Nov 7;9(11):e111969.
- Pickering AJ, Boehm AB, Mwanjali M, Davis J. Efficacy of waterless hand hygiene compared with handwashing with soap: a field study in Dar es Salaam, Tanzania. Am J Trop Med Hyg [Internet]. 2010 Feb [cited 2016 Dec 27];82(2):270–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20134005
- Widmer AF. Replace hand washing with use of a waterless alcohol hand rub? Clin Infect Dis [Internet]. 2000 Jul [cited 2016 Dec 27];31(1):136–43. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10913411
- Harnoss JC, Brune L, Ansorg J, Heidecke C-D, Assadian O, Kramer A. Practice of skin protection and skin care among German surgeons and influence on the efficacy of surgical hand disinfection and surgical glove perforation. BMC Infect Dis [Internet]. 2014 Dec 10 [cited 2016 Dec 27];14(1):315. Available from: http://bmcinfectdis.biomedcentral.com/articles/10.1186/1471-2334-14-315
- Haidegger T, Lehotsky A, Rona P, Pethes R, Szeremy P, Szilagyi L, et al. In the Footprints of Semmelweis: A Multi-Institutional Study on the Efficacy of Hand Rubbing. Am J Infect Control [Internet]. 2016 Jun [cited 2017 May 7];44(6):S72–3. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0196655316300876
- Colombo C, Giger H, Grote J, Deplazes C, Pletscher W, Lüthi R, et al. Impact of teaching interventions on nurse compliance with hand disinfection. J Hosp Infect [Internet]. 2002 May [cited 2017 May 7];51(1):69–72. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0195670102911989
- Graf K, Chaberny IF, Vonberg R-P. Beliefs about hand hygiene: A survey in medical students in their first clinical year [Internet]. Vol. 39, American Journal of Infection Control. 2011 [cited 2017 May 7]. Available from: https://www.sciencedirect.com/science/article/pii/S0196655311000927
- Scheithauer S, Haefner H, Schwanz T, Lopez-Gonzalez L, Bank C, Schulze-Röbbecke R, et al. Hand hygiene in medical students: Performance, education and knowledge. Int J Hyg Environ Health [Internet]. 2012 [cited 2017 May 7];215(5):536–9. Available from: https://www.sciencedirect.com/science/article/pii/S1438463912000284
- Buffet-Bataillon S, Leray E, Poisson M, Michelet C, Bonnaure-Mallet M, Cormier M. Influence of job seniority, hand hygiene education, and patient-to-nurse ratio on hand disinfection compliance. J Hosp Infect [Internet]. 2010 [cited 2017 May 7];76(1):32–5. Available from: https://www.sciencedirect.com/science/article/pii/S0195670110001192
- Donlon A. Hand hygiene compliance Item type Article. J Epi Insight Downloaded. 2009;10(7).
- Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. In: Gould DJ, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2010 [cited 2017 May 7]. Available from: http://doi.wiley.com/10.1002/14651858.CD005186.pub3
- Legler R, Bull M, Bell A, Johnson C, Dums T, Larson K. Hand hygiene compliance. Soc Nucl Med Annu Meet Abstr [Internet]. 2008 [cited 2017 May 7];49(Supplement 1):426P. Available from: http://jnumedmtg.snmjournals.org/cgi/content/meeting_abstract/49/MeetingAbstracts_1/426P-b
- Zingg W, Haidegger T, Pittet D. Hand coverage by alcohol-based handrub varies: Volume and hand size matter [Internet]. Vol. 44, American Journal of Infection Control. 2016 [cited 2017 May 7]. Available from: https://www.sciencedirect.com/science/article/pii/S0196655316306903
Appendix 1: Questionnaire Provided to Subjects













[…] infectious diseases, but the risk can be mitigated through an appropriate hand hygiene regimen. In our study, participant attitudes towards hand hygiene and the efficacy of hand disinfection with an […]
[…] a peer-reviewed publication of the findings within 3 months. We also performed an evaluation of hand disinfection using the Semmelweis System, which was a real-world clinical study of public behaviours conducted through multiple hospital and […]
[…] Evaluation of Hand Disinfection using the Semmelweis SystemReal world clinical study of public behaviours conducted through multiple hospital and university settings. Our team developed and wrote the IRB submission and methods, conducted the study, authored the paper, submitted for peer review and published the findings all within 4 months.Other notable deliverables included: Deep Dive Podcast interview, Showcase events in Buffalo and Toronto, Trials and Pilots, USA and Canada conference support.View Study: https://infectioncontrol.tips/2017/06/01/evaluation-his-system […]