While mycobacteria are well-known causes of tuberculosis (TB) and leprosy, many other species, variously called ‘nontuberculous mycobacteria’, ‘atypical mycobacteria’ and ‘mycobacteria other than tuberculosis’, are emerging pathogens of global significance. In contrast to the causes TB and leprosy, such species come from soil and water. Therefore, the term ‘environmental mycobacteria’ (EM) is used here to signify the environment as their primary habitat. Potting soil, hot water tanks, water coolers, ice machines, humidifiers, potable water distribution systems and other sites with stagnant water are among their reservoirs indoors. Thus, they lurk virtually everywhere inside our homes and hospitals (Lande et al. 2019). Figure 1 shows how exposure to EM can occur.
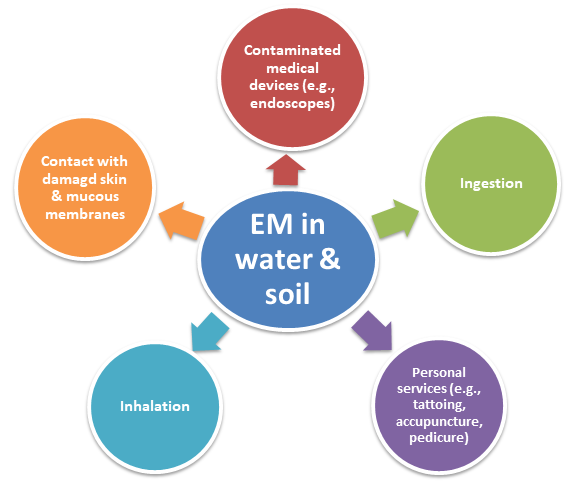
Figure 1. Possible means of human exposure to EM in water and soil
EM are a good example of ‘perikairots’ (Sattar 2013), which are environment-based opportunists. While they are particularly dangerous to the health of those debilitated by age, AIDS, cystic fibrosis (CF) or chronic obstructive pulmonary disease (COPD), otherwise immunocompetent persons can also succumb to them. Notably, EM are not known to cause secondary cases of infection!
Table 1 lists examples of such species and the infections they can cause.
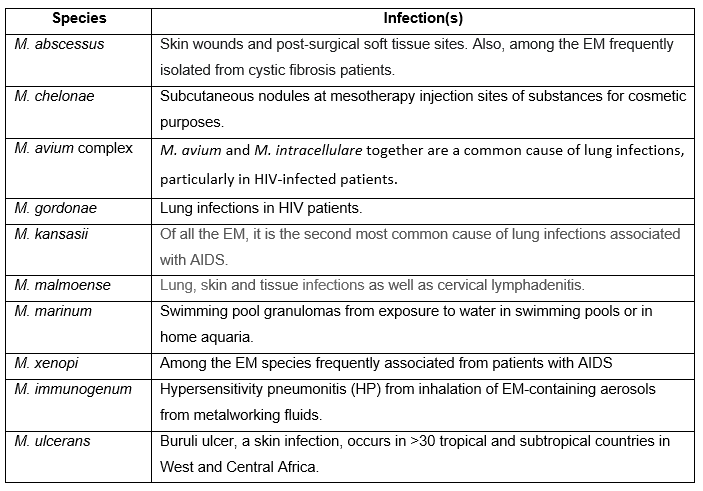
Table 1. Some examples of EM and the infections that they can cause in humans
Testing chemicals for their mycobactericidal activity
The genus Mycobacterium contains aerobic bacilli with a waxy coating, requiring ‘acid-fast’ staining for microscopy. They are also generally more challenging to culture while many pathogenic species requiring several weeks of incubation for visible growth. Therefore, standards-setting organizations such as ASTM International and AOAC International have separate methods for testing chemicals for their mycobactericidal activity (Sattar 2013). Interestingly, such testing focused not only on their tuberculocidal activity, but also as an indicator of a formulation’s ability to inactivate the hepatitis B virus, which remains refractory to culture in the lab. However, the continuing emergence of EM as human pathogens has now widened the need to test environmental surface as well as medical device disinfectants. This widening of the focus also requires that the term ‘tuberculocidal’ be replaced with a more inclusive and scientifically valid term ‘mycobactericidal’.
Features of EM as human pathogens are summarized in Table 2.
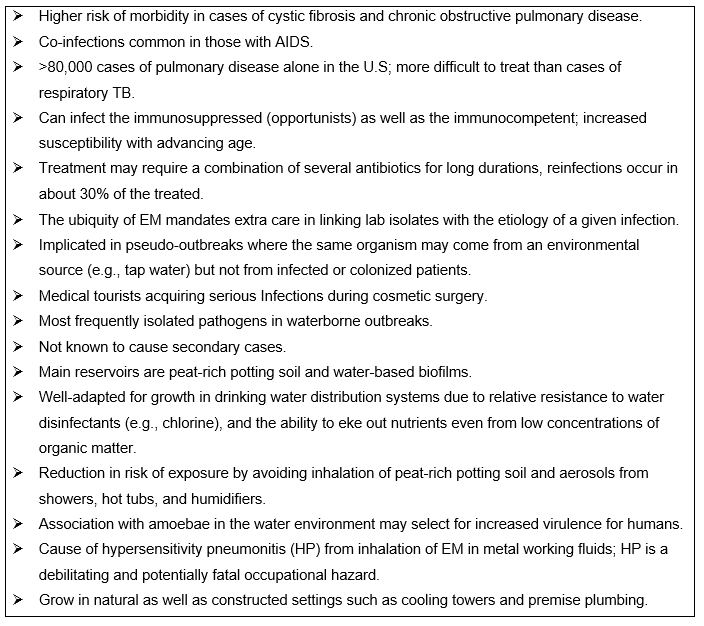
Table 2. Features of EM as human pathogens
https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/nontuberculosis-mycobacteria/learn-about-ntm.html
As indoor air is the primary vehicle for the spread of respiratory TB and EM, protecting air quality is crucial to reduce their airborne spread. Similarly, proper disinfection of heat-sensitive medical devices, another important aspect of routine infection prevention and control, aims to address the threat from both TB and EM. In this context, the choice of a surrogate for disinfectant testing is still under debate. Testing using M. bovis, required for regulatory approval, is quite challenging as the organism not only takes several weeks to grow in the lab, but its behavior also is often unpredictable. M. terrae is one among the current favorites because it grows nearly twice as fast as M. bovis with a consistent growth pattern along with a general disinfectant resistant profile predictive of that of the tubercle bacillus.
Further Reading
Falkinham J.O. 3rd. (2016). Current epidemiologic trends of the nontuberculous mycobacteria (NTM). Curr Environ Health Rep. 3:161-167.
Gebert, MJ. et al. (2019). Ecological analyses of mycobacteria in showerhead biofilms and their relevance to human health. mBio. 2018 Sep-Oct; 9(5): e01614-18.
Halstrom S. et al. (2015). Review: Environmental mycobacteria as a cause of human infection. Int J Mycobacteriol. 4:81-91.
Lande, L. et al. (2019). Mycobacterium avium in community and household water, suburban Philadelphia, Pennsylvania, USA, 2010–2012. Emerg Infect Dis. 25: 473-481; 2019.
Sattar, S.A. (2013). Testing of chemicals as mybactericidal agents. In Principles and Practice of Disinfection, Preservation and Sterilization. Blackwell Publishing Ltd., Oxford, U.K. Pages 131-141.
CREM Co Labs
CREM Co is a contract and R&D laboratory uniquely positioned to provide value to the infection prevention and control (IPAC) industry as well as those working in health-related environmental microbiology and molecular biology.
CREM Co has the expertise for handling all major classes of pathogens. It can assess disinfectants and antiseptics using internationally accepted test protocols under good laboratory practice compliance. Please visit www.cremco.ca for more details.