THIS DOCUMENT IS NO LONGER UPDATED
Evolving Document – Last Updated: October 30, 2020 –
With the current outbreak, it is important to discern what are the real facts, and what is sensationalized by the media. Refer back to this article for scientifically-backed evidence as it becomes available. If you have additional information, please send any peer-reviewed or public health agency approved information to [email protected]. If you would like clarity on any topics, please contact us at [email protected].
This live document covers:
- What is Coronavirus?
- What is the COVID-2019?
- Countries Affected
- What is a Pandemic
- Transmission
- Symptoms
- Testing
- Prevention
- Infection Control (Surface Disinfection methods)
- References
What is Coronavirus?
This is the name for a family of viruses which are mainly characterized for have a positive-stranded RNA genome, and are incased in a membranous envelope (Geller et al, 2012). In recent history, it has been the extensively studied in, as this virus family was responsible for the SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome) outbreaks in 2003 and 2012, respectively.
What is COVID-2019 or Coronavirus disease?
The Coronavirus originally identified in Wuhan is categorized as a novel Coronovirus, which the World Health Organization (WHO) has named COVID-2019. Multiple patients presenting with symptoms of a severe respiratory infection (pneumonia) originating from Wuhan, China were identified in late 2019, and were confirmed by electron microscopy and genome sequencing to be a coronavirus. Given the current spread of the infection, it is likely that the virus is spread through respiration (airways) (WHO, 2020). The origin of the virus is unknown, but current research suggests it is zoonotic (animal-borne) and crossed the species barrier to infect humans.
As of June 15, 2020 the WHO states:
- Globally, about 3.4% of reported COVID-2019 cases have died. By comparison, seasonal flu generally kills far fewer than 1% of those infected
- COVID-2019 causes more severe disease than seasonal influenza
Countries Affected:
Data Updated via Johns Hopkins University
SOURCE: Johns Hopkins Center for Systems Science and Engineering
What is a Pandemic?
A ‘Pandemic’ is an epidemic (cluster of diseases in a region) that has spanned to cross multiple continents and is essentially considered to be worldwide. This is especially harmful as it indicates that infection control measures to keep the illness isolated to a region was unsuccessful. A Pandemic DOES NOT indicate that the disease has mutated, become more dangerous, or changed in any appreciable manner. This is merely an indication of regional spread.
As COVID-2019 approaches pandemic status, multiple countries are implementing pandemic measures. These may include, but are not limited to: increasing resources to develop treatments for the disease, increasing resources to improve screening measures to limit the spread of the disease, possibly limiting travel to potential sources of the diseases, and ensuring that the country has the resources to combat the likely increasing number of disease cases. By taking local action, this can help to combat the spread of the disease worldwide. For many countries, pandemic response plans are already developed and just need to be implemented when the time comes. In preparation for this, many countries have already announced that they are implementing their Pandemic Response.
Please contact your local Public Health Agency or Public Health Organization to find out your country’s specific Pandemic Response Guidelines.
Transmission
According to the CDC: COVID-19 is thought to spread mainly through close contact from person to person, including between people who are physically near each other (within about 6 feet). People who are infected but do not show symptoms can also spread the virus to others.
– spreads very easily from person to person
– most commonly spreads during close contact
– can spread by airborne transmission
– can spread by contaminated surfaces
– rarely spreads between people and animals
CDC: How COVID-19 Spreads: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html
Symptoms
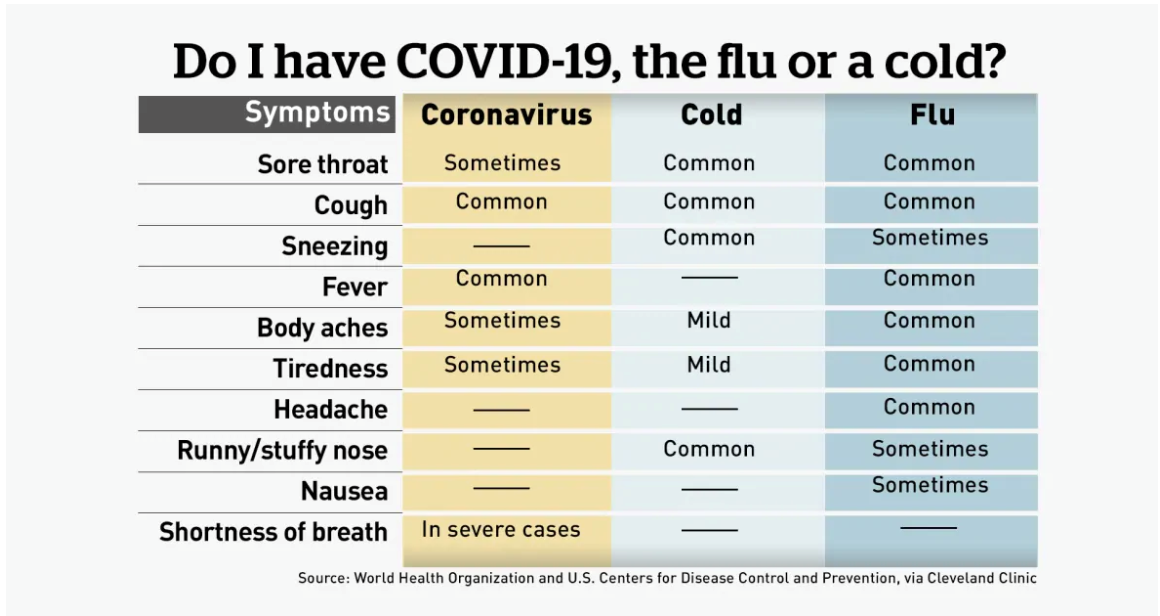
Symptoms will vary in severity. Current general symptoms include fever, difficulty breathing, , severe cough, and pneumonia in severe cases. The symptoms are similar to the seasonal cold and flu but should be monitored carefully before establishing a diagnosis.
If you or anyone around you presents with these symptoms, it is recommended that you practice self-isolation. Current evidence suggests that patients are contagious 2 days prior to, and up to 14 days after symptoms develop. All individuals within the home should self-quarantine, given the likelihood of within-home transmission. Please contact your local health authority for further directions on potential testing and reporting requirements.
Testing
Currently, the genome is sequenced, and available on the World Health Organization website for reference. There are NO commercial RT-PCR, immunoassays or culture assays available for immediate testing yet. Please refer to the technical guidance documents from the WHO for up to date information on validated testing methods. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
Prevention
Given the evidence available, it is recommended to individuals to prevent infection by nCOVID-2019 with strategies developed for both the SARS-CoV and MERS-CoV. Without a known animal origin of the virus, there is currently no indication for eliminating any animal sources to prevent further zoonotic transmission. Previous outbreaks were likely a result in failure/breaches in Infection Prevention and Control practices (WHO, 2020).
Hand washing – It is recommended that all individuals that are in public spaces wash their hands as frequently as possible for a minimum of 20 seconds with soap and copious amounts of water. In the event a suitable water source is not available, please use hand sanitizers with a minimum alcohol content of 60%. It is recommended to avoid touching high contact surfaces (areas which may be touched or are accessible to many people) when possible, and to avoid touching your face as much as possible.
Masks – It is recommended that all individuals wear a mask when they are in a public space which may come into contact with other individuals. The use of masks by everyone reduces the spread of droplets which may contain the virus particles. Commercial masks made of a cloth or cloth-like material is recommended. Home-made masks should be made out at least a double layer of cotton, and appropriately sized for the person.
All cloth face masks should:
- fit snugly but comfortably against the side of the face
- completely covers the nose and mouth
- is secured with ties or ear loops
- includes multiple layers of fabric
- allows for breathing without restriction
- can be laundered and machine dried without damage or change to shape
Masks are not recommended for persons under the age of 2, or anyone who has difficulty breathing while wearing the mask or is unable to remove the mask without assistance.
Vaccines – No current vaccines are available, but candidate vaccines are in development, which may assist in preventing development of a 2019-nCoV vaccine.
Personal Protective Equipment- Employ personal protective equipment for the prevention of airborne disease. Employ the use or aerosol-reducing practices.
- Gloves should be ideally be nitrile, and have long cuffs.
- They should be: EU standard directive 93/42/EEC Class I, EN 455; EU standard directive 89/686/EEC Category III, EN 374; ANSI/ISEA 105-2011; ASTM D6319-10; or equivalent
- Masks (surgical) should have high fluid resistance, good breathability, internal and external faces should be clearly identified, structured design that does not collapse against the mouth (e.g. duckbill, cupshaped)
- EN 14683 Type IIR performance ASTM F2100 level 2 or level 3 or equivalent;
- Fluid resistance at minimum 120 mmHg pressure based on ASTM F1862-07, ISO 22609, or equivalent
- Breathability: MIL–M-36945C, EN 14683 annex C, or equivalent
- Filtration efficiency: ASTM F2101, EN14683 annex B, or equivalent
CDC: Use of Masks to Help Slow the Spread: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html
- Gowns should be single use, fluid resistant, disposable, length mid-calf to cover the top of the boots, light colours preferable to better detect possible contamination, thumb/finger loops or elastic cuff to anchor sleeves in place.
- Option 1: fluid penetration resistant: EN 13795 high performance, or AAMI PB70 level 3 performance or above, or equivalent
- Option 2: blood borne pathogens penetration resistant: AAMI PB70 level 4 performance, or (EN 14126-B) and partial body protection ( EN 13034 or EN 14605), or equivalent
- Face Shields should be made of clear plastic and provides good visibility to both the wearer and the patient, Adjustable band to attach firmly around the head and fit snuggly against the forehead, Fog resistant (preferable), Completely cover the sides and length of the face, May be re-usable (made of robust material which can be cleaned and disinfected) or disposable.
Infection Control (Surface Disinfection Methods)
Given the rapid spread of the illness, all suggested cleaning and disinfection methods are based on the efficacy of these products against similar viruses. As more direct evidence is published, it will be updated on this list. Contact the manufacturers and your local public health agency for local regulations and use instructions. Brands are listed only for reference and do not represent a complete list. Products are listed in alphabetical order and not in order of efficacy, as it is still inferred at this point. If there are any omissions, please contact [email protected] identifying the evidence, including registration where applicable.
Only relevant organisms to Coronavirus are listed.
DOWNLOAD THE LIST:
Click here to download PDF version: COVID-19 Surface Disinfection Methods
| Product | Commercial Name(s) | Registration | Efficacy* | Notes |
| Accelerated Hydrogen Peroxide | Oxivir (Diversey) | EPA | Human coronavirus, Hep C, Influenza A, Swine Influenza A (H1N1) | 60 second contact time |
| Ethanol | Ethanol | Not required | Most viruses | |
| Hydrogen Peroxide/Peracetic Acid | Virasept (Ecolab Inc) | EPA | Human coronavirus, Hep C, Influenza A, Swine Influenza A (H1N1) |
|
| Isopropyl alcohol | Klercide (Ecolab) | EPA | ||
| Quaternary Ammonium Compounds (Quats) | -Condor2 (WM –Barr)-Stepan Spray Disinfectant- Sterilex Ultra Step (various)- Lysol Disinfectants (various)- Clorox Disinfecting Cleaner (various)-Lonza Formulations (various)-Peak Disinfectants (North American Infection Control)-Sani-Prime Germicidal Spray (Professional Disposables International) |
EPA | ||
| Silver dihydrogen citrate | Pure Hard Surface (Clearly Better) | EPA | Human coronavirus, Rhinovirus, Rotavirus, Respiratory Syncytial Virus (RSV), Hep B, Hep C, Influenza A (H1N1); Swine Influenza A (H1N1) | 30 to 60 second contact time for viruses |
| Sodium dichloroisocyanurate
(NaDCC tablet) |
Klorkleen (Kersia)
PurTabs/Pur:One (EvaClean) Defender (Lighthouse) C.diff tablet (3M) BruTabs (Brulin) |
EPA | Hep A, Hep B, Porcine Epidemic Diarrhea virus (PEDs), Influenza Virus H1N1, Norovirus | Kill time of 1 min at 4,000 PPM |
| Sodium hypochlorite | -Bleach
-Clorox Healthcare Fuzion (Clorox) -Avert (Diversey) |
EPA | Most enveloped viruses | |
| Ultraviolet C (UVC) | Surfacide UV | Not Required | MERS-CoV, Pseudorabies virus (PRV), Porcine reproductive and respiratory syndrome virus (PRRSV), Porcine epidemic diarrhea virus (PEDV), Bovine viral diarrhea virus (BVDV), Classical swine fever virus (CSFV), Swine influenza virus (SIV) | >5 log10 reduction in 5 minutes |
| Ultraviolet C (UVC) | Sanuvox (PrescientX) | Not Required | MERS-CoV, Pseudorabies virus (PRV), Porcine reproductive and respiratory syndrome virus (PRRSV), Porcine epidemic diarrhea virus (PEDV), Bovine viral diarrhea virus (BVDV), Classical swine fever virus (CSFV), Swine influenza virus (SIV) | >5 log10 reduction with >20 mJ/cm2
UV dosage for most viruses |
| Chlorine dioxide (ClO2) | Prokure V (Prokure) | EPA | Hepatitis A, Rhinovirus type 37, Coronavirus, Influenza A, Influenza A. |
*Only relevant organisms to Coronavirus are listed. Please contact the manufacturers and your local public health agency for local regulations and use instructions.
**A full list of products identified by the EPA can be found at https://www.epa.gov/sites/production/files/2020-03/documents/sars-cov-2-list_03-03-2020.pdf
References:
- Centre for Disease Control (2020) Coronavirus. Retrieved 27 Jan, 2020. https://www.cdc.gov/coronavirus/index.html
- Geller, C., Varbanov, M., & Duval, R. E. (2012). Human coronaviruses: insights into environmental resistance and its influence on the development of new antiseptic strategies. Viruses, 4(11), 3044-3068.
- World Health Organization (2020) Coronavirus Retrieved 27 Jan, 2020. https://www.who.int/health-topics/coronavirus
The novel coronavirus situation is evolving and dynamic. The information presented on this page, journal and website does NOT replace the guidance and direction of your local government and health authority. Readers are advised to contact their local government and regional health authorities for specific instruction on all the topics mentioned.












