Abstract:
In non-hospital settings, health care professionals face the challenge of a constantly evolving environment. The specialists at Médecins Sans Frontières /Doctors Without Borders are deployed to areas where clinics and hospitals are not available, or unable to accommodate the needs of the community. In this article, two front line workers discuss some of the bigger challenges they face in these situations.
Main Article:
Sharla Bonneville is a television producer. She also leads another life you might not suspect. She is a non-medical, project-based water and sanitation manager and logistician who serves the Canadian office of Médecins Sans Frontières (MSF) — better known in some places as Doctors Without Borders. The mission of MSF is to provide care and medical treatment to vulnerable populations, often in emergency contexts, such as wars, epidemics and natural disasters, and to bear witness to what they have seen. Through this type of as-needed work, Sharla has been called into action in far-flung locations, directly impacting the success of critical MSF projects, and has played a part in saving many lives.
Through her work with MSF, Sharla has witnessed incredible suffering and despair caused by infectious diseases and has faced seemingly insurmountable challenges in providing help and hope to vulnerable communities. She finds strength and purpose in even the smallest of infection prevention victories:
I remember sitting with a bunch of local people who were working as medical centre cleaners, trying to get them to understand how diseases spread. They didn’t really understand, and they weren’t following protocols correctly, which was putting everyone — even their own families — at risk. Because I didn’t speak their language, I showed them a pictogram, pointing to illustrations and explaining, “When a fly lands on poo, then this happens, and then you get sick.” One day, one of the cleaners came up to me and said there had been flies all over the meat at the market. She told the man there to cover the meat, because it was going to make people sick. She finally understood! And she was able to teach someone else. That’s what it’s all about.
Preventing the spread of disease in the modern world can be unbelievably challenging in a multitude of ways. More than ever before throughout history, people are traveling long distances and unintentionally carrying disease across borders. Civil unrest and war have led to an increasing number of people being displaced and forced to live in close, temporary quarters. Coupled with the growing resistance of bacteria to antibiotics, infection prevention has become one our foremost challenges in modern society.
While hospitals and universities play an important role in the fight against the spread of diseases, some of our greatest challenges, and therefore opportunities for innovation, are in places where conditions are less than ideal. Places like Uganda and Turkey that have seen an insurgence of refugees from war-torn neighbours; or places like Sierra Leone and Mali, where the medical needs are high for diseases like Ebola and malaria, but the access to patients is limited by geography, poverty and political unrest. In these places, disease tends to spread more frequently and more quickly. If communication is poor among health professionals, the practices to prevent infections quickly dissolve, resulting in the mismanagement of resources, and that can have deadly consequences.
Dr. David Olson knows as well as anyone the challenges of infection prevention in the field. He is a member of the MSF-USA management team and also an organizer and field medic. Working with a team of specialists, David has focused his efforts on studying infectious disease/antibiotic resistance, tropical medicine/malaria, and health information systems.
Like other medical practitioners, Dr. Olson had many career options, but ultimately chose field medical service. “I decided I wanted neither to be an academician nor in private practice, but rather work with and for those who do not benefit from the abundance and good fortune that comes with the luck of where and to whom one is born.”
For most of us, these conditions and potential fatal outcomes are daunting. The idea of traveling to unfamiliar places, exposing ourselves to horrifying diseases and facing nearly impossible odds to save lives is the stuff of novels and news headlines, but for people like Sharla and Dr. Olson, it is an exciting and meaningful reality they are well-prepared to face. Through impressive planning and organization, MSF staff, both medical and non-medical, have become experts in staging, supplying, building and implementing field medical centres to fight disease. MSF provides a multitude of articles, handbooks, videos, training materials and other resources to help healthcare workers throughout the world.
The MSF Field Infection Prevention Machine
Infection prevention on a worldwide scale begins with a strong infrastructure. Over the past 43 years, MSF has built an impressive, inter-connected system of staff, strategies, protocols and resources for responding to worldwide health emergencies. The organization consists of half medical professionals and half nonmedical specialists. The nonmedical specialists include water and sanitation specialists, financial coordinators, human resources coordinators and logistics personnel.
“It’s great if you have a medical team,” Sharla explained, “but if you have no cars, lighting, clean water, medicine and beds, you won’t get far. We are successful because we all work together and we have the ability to adapt to the context of each project.”
The MSF infrastructure and organization is focused on supplying people and resources quickly and effectively, as well as getting the logistics correct, so more lives can be saved. A great deal of time and attention is paid to establishing medical and nonmedical protocols and training staff to follow them.
MSF reference and training materials are open to the public, including emergency health care workers from other organizations. Access reference books via www.refbooks.msf.org.
Once the need for MSF assistance is identified, the first step is to bring together the necessary resources and teams. There is usually a coordination team in the capital city of the destination country, in addition to project-level medical and logistical coordinators.
A field management team handles onsite coordination, with a backup team in an assigned operational centre. There are eight operational centres around the world. Sharla has a contract with MSF Canada, and Dr. Olson serves as cholera specialist and contributes to overall strategic planning and implementation oversight of medical activities for MSF-OCP (Médecins Sans Frontières – Operations Centre of Paris).
According to Dr. Olson, it is important that dedicated personnel with a high level of expertise be charged with infection prevention. “Of primary importance is that these positions are not included in the job description of someone already working with other responsibilities. That never works. Ideal candidates are committed to the [need for infection prevention], persistent and firm, and can gain and maintain the respect of local staff, who may be skeptical.”
Every situation is different. The most challenging projects are those that must be built from scratch. Dr. Olson explains: “In the early stages, a site is not aided by electronic medical records, does not benefit from a large armamentarium of antibiotic choices, infrequently has reliable culture and drug sensitivity, operates in an environment that has little or no background information on prevailing drug resistance patterns, involves hospitals that are ventilated by air from the outside and frequented by flying insects, with highly specialized antibiotics, sometimes of dubious quality freely available on the open market, and on and on.”
Even if staff have training, they might not have worked in a developing country before, and they may not fully realize the impact of certain aspects of the work, such as supply chain limitations, working without proper equipment and getting locals to understand the seriousness of the situation. Standardization helps, but Sharla explains that staff must be ready for anything.
The Ebola outbreak of 2014 is a good example of how things can change quickly. “Previous outbreaks were based on 10 beds,” Sharla said, “but in one of the centres last year there was a need for more than 400 beds. No one was thinking on this level.”
MSF standards and protocols are constantly being reevaluated and updated for this reason. Sharla also points out that many of the standards are minimum. For example, it is standard to allot a minimum of twenty litres of water per person in a refugee camp. That doesn’t mean they should only receive twenty litres. Every patient and every ward is different.
Challenges in the Field for Infection Prevention Professionals
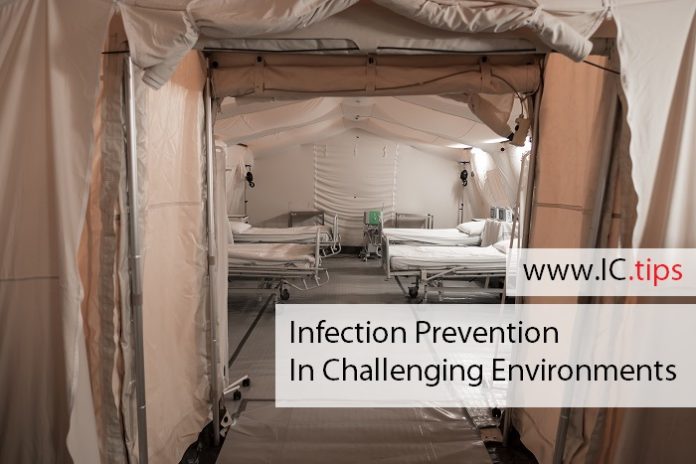
All aspects of a project deployment present challenges to infection prevention. Sharla has observed how project settings can vary widely. “You can be doing a clinic under a mango tree, or you can be in a tent, or you also could be in a state-of-the-art hospital. You have to roll with it. You have to arrive and get to work. Sometimes you have to do the best that you can do with what you have at the moment. However, the principles of our operation stay the same, and that’s the point behind everything in infection control.”
Healthcare services at an MSF site are based on assessment, standards, protocols, and context. “We start with the lowest hanging fruit,” said Dr. Olson, “such as beds spaced a correct distance, separate wards for patients infected with drug-resistant bacteria, washing hands between each patient we see, proper sterilization of medical equipment, and antibiotic choices.”
Antibiotics are often misused in smaller, isolated communities, which makes it more difficult to treat patients who really need them. In field emergency situations, the inability to treat resistant strains of disease can lead to increased morbidity.
Cultural differences also must be overcome before good infection prevention protocols can be stabilized. Outreach personnel work with community leaders to build trust and educate local residents. Many nontraditional educational activities have been developed to help (often uneducated) citizens understand the dangers of infectious diseases and preventative actions.
To help illustrate transmission of a virus or germs, exercises are used to visually demonstrate how easy it is to spread disease. Local staff might be given gloves that have been covered with glitter and then be asked to carry on normally to see how the glitter ends up on everything that is touched.
Infection Prevention: A Global Concern
In the eyes of Sharla, there is a big difference between infectious disease outbreaks and other MSF projects. The invisibility of diseases causes logistical and perceptional difficulties. “In other contexts, you can see what’s happening. In a war zone, you can see the conflict and hear the fighting. You can see malnutrition or the red bumps of measles. With Ebola, for example, it was hard to comprehend where the problem was coming from,” she explained. “Some people were becoming very sick, very quickly and then dying. It was difficult to connect the reality to what was happening and it was hard to believe the level of personal protective equipment (PPE) that needed to be worn against this invisible virus.”
Even in a non-medical setting, infectious diseases are invisible until people become very sick. As globalization makes the world smaller, the need for infection prevention measures emerges as one of the most important medical objectives in every community. Frontline personnel in organizations such as MSF are finding solutions in the most difficult of circumstances and are leading the charge in understanding the true impact of infectious diseases. With their work and insights, we will become better equipped to continue studying, planning and preparing for future infectious outbreaks.
“Bearing witness to what we see” is as important a part of the mission of MSF as is providing medical and logistical services. Personnel in the field, such as Sharla and Dr. Olson, who have intimate knowledge of the inner workings of infection prevention, can share their passion and knowledge to help others learn and implement the same protocols, to meet the same challenges, to save lives and to make a difference.