Peer Reviewed
Abstract:
This study determined the attitudes toward utilization of insecticide-treated bed nets among pregnant women and children under-five in the Ikwerre Local Government Area (LGA) of River State, Nigeria. Questionnaires were administered to 364 pregnant women and mothers/caretakers of under five children attending clinic session at selected health centre and hospitals in the LGA. Over eighty percent (80%) of the study population had one form of a mosquito net at home. Upon observation only 27.7% of the nets could be seen in homes; of which 11.1% were hung appropriately. The main source of acquisition of the insecticide-treated nets (ITNs) was from the antenatal clinic (42%). Knowledge of the use of mosquitoes bed nets (MBNs) as a preventive measure against malaria had no significant effect on actual use of the net by the study population It is suggested that government should increase its efforts at improving the awareness of the benefits of ITNs use and ensure free distribution accompanied by participatory approach.
Introduction:
Malaria causes significant morbidity and mortality amongst pregnant women and children under 5 in Africa (The World Bank, 2006). Among the approaches for control of this disease, the use of insecticide treated bed nets (ITN) has been accredited as a cost effective methods in prevention against malaria and has been found to significantly decrease morbidity and mortality amongst these groups of individuals (“KHN Morning Briefing,” 2009.). This study determined the attitudes toward utilization of insecticide-treated bed nets among pregnant women and care takers of under-five children in the Ikwerre Local Government Area(LGA) of River State, Nigeria. Results of this research will aid governmental and non-governmental organizations to put in place proper strategies to address/promote the use of ITNs and thus reduce morbidity and mortality due to malaria; particularly among vulnerable groups, such as children and pregnant women.
Hypothesis:
The attitudes towards use of ITNs among pregnant women and for caretakers of children under five is significantly dependent on the sociocultural factors.
Materials/Methods of the interventions:
The descriptive survey was disseminated to women who are pregnant and people who are caretakers of children less than five years in the Ikwere local Government Area that were attending clinic session at selected health centre at hospitals in the LGA. An observational checklist completed by healthcare providers was also used to collect information that will complement data gotten for the questionnaire.
Results Of Data Analysis
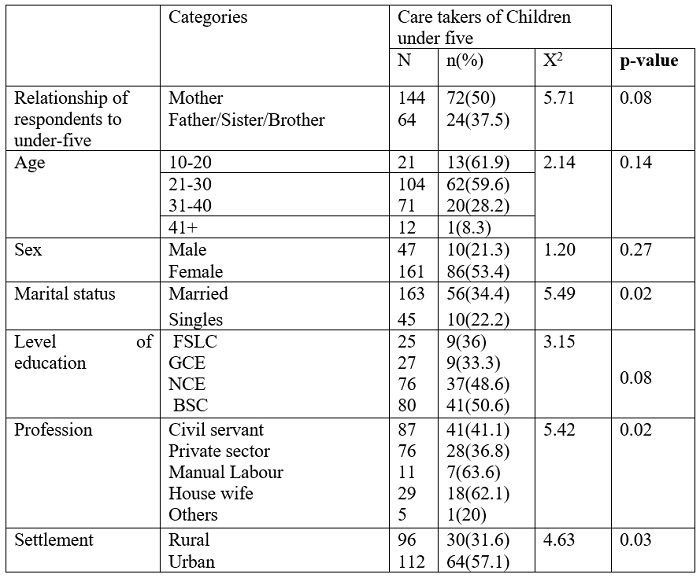
Demographic Characteristics Participants
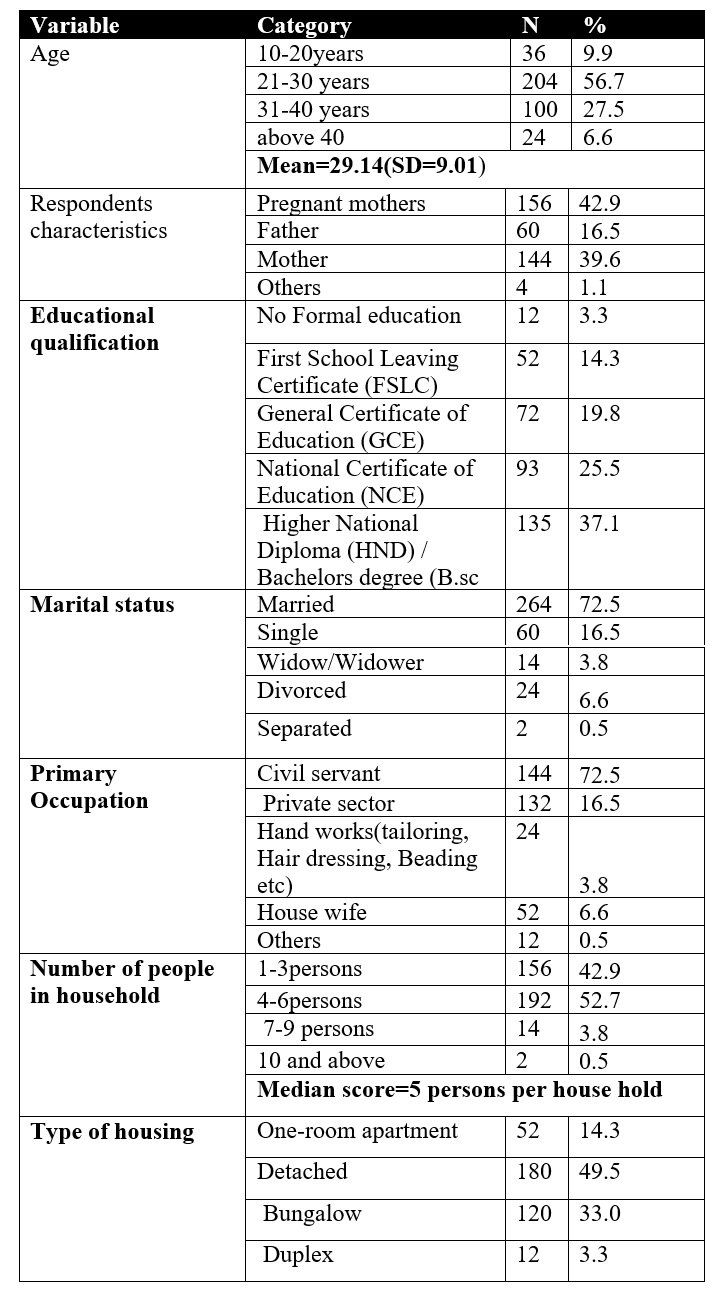
The majority of respondents were pregnant women (42.9%) or mothers (39.6%). The ages of the respondents ranged from 13 to 73 years with mean age being 29 years (Table 1). With regard to the level of education, a majority of the respondents (37.1%) had a Higher National Diploma (HND) or a Bachelors degree (B.Sc), and a minority of 3.3% had no formal education. Seventy-two percent of the respondents were married. Respondents were involved in very many different activities including largely, civil service duty, private jobs like businesses, manual labour including tailoring and hair dressing, and others like homemakers and students.
Table 1: Demographics of Participants
Ownership and source of acquisition of Mosquito Bed Nets (MBNs)
71.2% pregnant women owned ITNs, and for children under five, 81.2% of the caretakers affirmed that the children used an ITN (Figure 1). In total, (77.2%) participants had a net while 22.8% did not.
Sources of MBNs acquisitions
The main source of ITNs were from antenatal clinics (ANC)/other hospital clinics (42%). Other sources of ITNs acquisitions to the study population were during health campaigns (21.4%), retail markets (11.4%), schools (8.5%), NGOs (8.4%) and churches (7.1%).
Knowledge of use of ITNs as a preventive measure
The respondents had a good knowledge of the utilization of ITNs as a preventive measure. Only 3% of the population said the ITNs are a bad/very bad preventive measure (Figure 1).
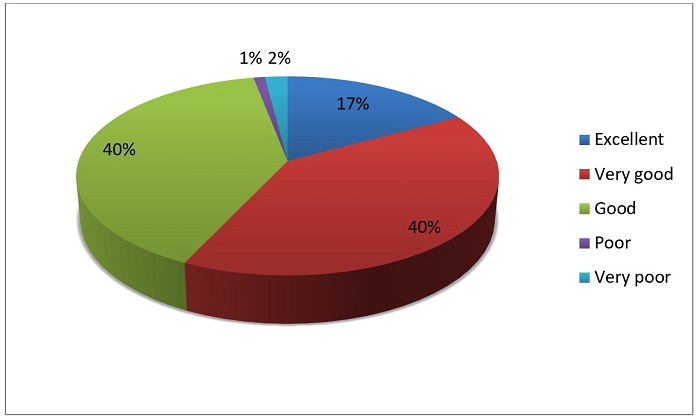 Figure 1: Notion of ITNS as a preventive measure against Malaria
Figure 1: Notion of ITNS as a preventive measure against Malaria
The proportions of respondents having a good level of knowledge on malaria decreased with age. A total of 90% of respondents 41+ years had a good level of knowledge, and decreased to 86% for 21-40 years and 76% for 13-20 years old respondents. Eighty-three percent (83%) of respondent with zero or primary level educationhad a good level of knowledge on malaria as opposed to 91% of secondary, high school, or university-level respondents. This difference was statistically significant (X2 = 6.60; p = 0.010). Equal proportions of females and males (88%) had a good knowledge on malaria.
Priority Household Members to sleep under MBNS
It was determined that 77.2% of the respondent were of the opinion that pregnant women and children under five should be giving priority to sleep under ITNs (Figure 2). Approximately 11.5% of respondents said children less than are more vulnerable and should be giving priority, while 5.5% said the sick should be given the priority to sleep under the ITNs. Only 5.8% stated that only pregnant women should be given priority to sleep under an ITNS.
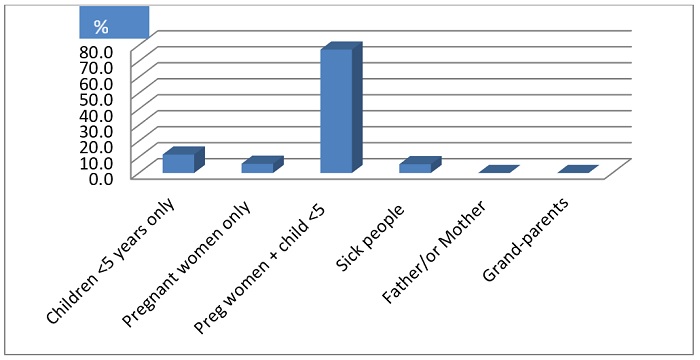
Figure 2: Priority Household Members to sleep under MBNS
Use of the ITN
Of the respondents,18.1% of respondents said they always made use of ITNs; of which 15.5% were pregnant women and 19.6% were children under five years of age. 13.2% of the population of study used the net solely in the rainy season. Fifty-eight percent of the study population had never made use of an ITNs while 10.7% used it occasionally (Table 2).
Table 2: Usage of ITN by pregnant woman/the child under five years
(N = number of respondents)
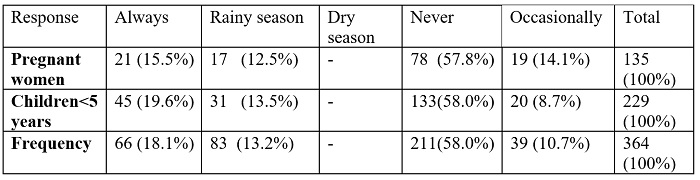
None of the respondents used MBNs solely during the dry season. The weather was deemed too hot and the use of MBNs would increase the temperate, making it uncomfortable to sleep. Those who used bed nets only in the rainy season said mosquito density increases during this period and therefore transmission of malaria is higher. Another reason for preferring the rainy season was that instead of the discomfort from heat experienced in the dry season, they would benefit from the warmth provided by MBN during the cold nights.
Infuence of demographic factors on the utilization of mosquito bed nets among caretakers for children less than five
The only factor associated with ensuring children under five sleeping under mosquito bed nets was the age of respondent (Table 3). Interestingly, utilisation of ITNs decreased with age. The majority (59%) of respondents below 30 years made use of the bed nets. The female care takers were 8.6 times more likely to use the bed nets than the male caretakers. However, the correlation was not significant (p= 0.27, X2=5.14). Fifty-seven percent of the urban population ensured that children made use of the ITNs. After adjusting for all other variables, children in urban settlements were two times more likely to sleep under ITNs compared to those of rural communities. Also there was no significant diference in the use of ITNs based on respondants educational background (P= 0.08, X2=3.15).
Table 3: The utilization of mosquito bed nets among caretakers of children under 5
Influence of knowledge of ITNs as a preventive measure agains malaria on the utilization of mosquito bed nets among caretakers of children under five
Surprisingly, knowledge about ITNs as a preventive measure against malaria had no effect on its utilization. Only 47.1% of those who perceived it as a good preventive measure regularly used it for their children. However, this was statistically insignificant (X2 = 9.52; p = 0.02).
Influence of demographic factors on the utilization of mosquito bed nets among pregnant women
Interestingly, only the respondents’ level of education significantly affected ITNs usage among pregnant women. Use of ITNs increased with increased educational status. Those with no formal education showed a very low use rate of 8.3% (Table 4). The proportion of pregnant women who slept under ITN was slightly higher among single women (43.6%) as opposed to 32.6% among the married (X2 = 6.13; p = 0.01). Pregnant housewives had the highest percentage (52.2%) of utilization of ITNs compared to pregnant women involved in out-of-home income generating activities. The proportion of pregnant women sleeping under MBN was highest in rural areas (38.6%).
Table 4: The utilization of mosquito bed nets among pregnant women
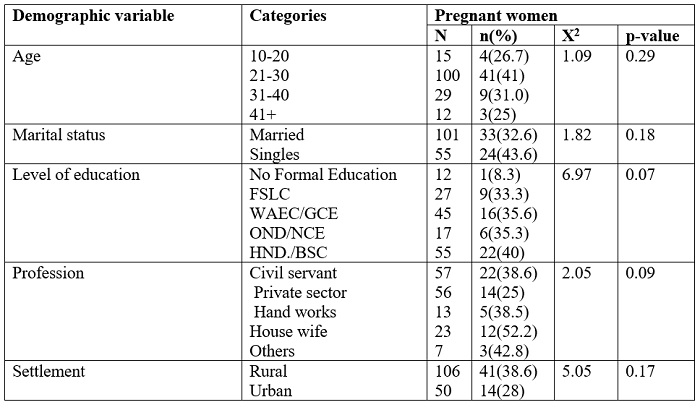
Sociocultural factors that could affect ITNs use among respondents
The participants of the study agreed that some socioeconomic factors could influence sleeping under ITNs. In table 5, it can be seen that the participants’ religious practices did not affect the use of the net. Some of the factors that negatively impacted the use of ITNs included: lack of accommodations/space, the belief that ITNs reduces airflow, increased heat when sleeping under the ITN, breathing difficulties, skin reaction to the chemical in the nets, and the inconvenience of tying the net up every day.
Table 5: Sociocultural Influence on ITN use
Overall, providing the ITNs for free was a common reason that could compel 29.2% of the respondents who have heard about ITNs to use it more regularly. The majority of the population of study (43.1%) said they could use the net if the weather is cool. While only 7.6% of the population who have the net said hanging it was a hindrance to usage.
Household Observations
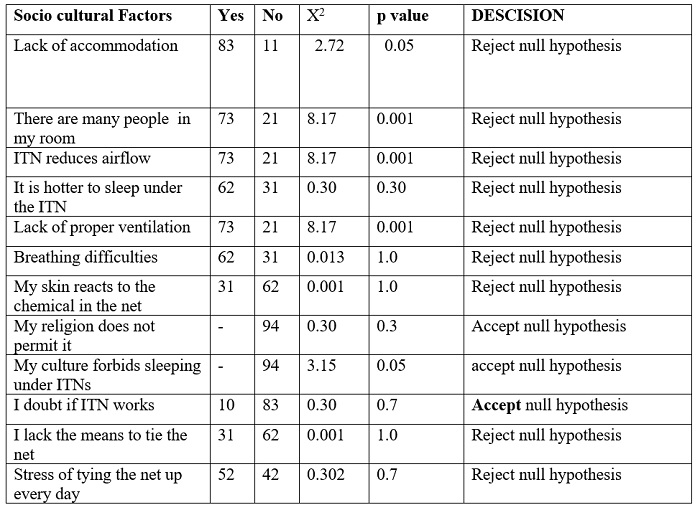
Observations made in the homes revealed the following: Of the 364 respondents, 101(27.7%) of homes actually utilized the ITNs. \Some respondents were resistant to showing the net to the researchers. Thirty-four (33.7%) of those hung over the bed had holes and tears (Figure 3). The ITNs were seen in different states of disrepair: 22(21.8%) were torn beyond effective-use, 2 (2%) were hung on the windows, 45(44.5%) were just folded and lying somewhere in the room (Figure 4a) and 20 ITNs were still sealed inside their packages (Figure 4b). Just 12 (11.8%) 0f the nets where hung properly without any fault detected. In many cases, the ITNs were being utilized for other purposes, including a drying rack for diapers (Figure 5). Most of the respondents’ rooms had poor ventilation, increasing the temperature. Most of the respondents had fans /air conditioning systems in their houses, but could not make use of them because of the irregular electrical supply in the area. Some of them stated that if they had consistent electricity at night to use their fan/air-conditioner, it would have made it more comfortable to use the net; especially in the dry season when temperatures are at their highest.

Figure 3: A torn mosquito bed net
(Pictures provided from Atenchong, 2014)
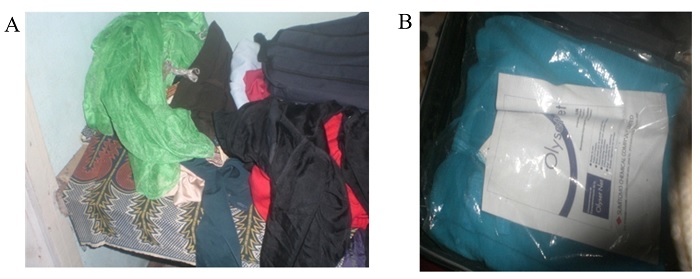
Figure 4: a) Mosquito bed nets stored among clothes in wardrobe
b) MBN sealed in original packaging.
(Pictures provided from Atenchong, 2014)

Figure 5: ITNs and MBNs were often utilized for other purposes,
including as a drying rack for diapers.
(Pictures provided from Atenchong, 2014)
Discussion:
This study examined the attitudes toward utilization of insecticide-treated bed nets (ITNs) among pregnant women and children under five in the Ikwerre local Government area (LGA) of Nigeria. Seventy-one percent of pregnant women owned and ITNs and 81.2% of caretakers of children owned at least one ITN. Of the total respondent population, 42.1% of the pregnant women made use of the ITN and 41.8% of the caretakers of children under five made use of the ITNs. Of those who used the ITNs, only 18% of the total population reported regular use of the ITNs regularly. This indicates that although a majority of the population owned an ITN, a great proportion of the vulnerable populations of the Ikwerre LGA were not regularly protected against malaria with ITNs. This implies that the burden of malaria morbidity and mortality among the vulnerable populations of Ikwerre LGA may continue to exist. This can be confirmed by Wendy et al (2010), who stated that although there appears to be a decline in the burden of malaria incidence in Africa, reports from Nigeria indicates that there is a rise with a reported increased incidence of severe malaria.
ITNs ownership and use in Nigeria have always been reported to be lower than in many of the other countries in the sub-region (Amoran et al 2011; Afolabi et al 2009; Tobi West et al 2011, Oresanya et al 2008; Erhun et al 2005; Ehijie et al 2007). This may be related to the poor attitude and practice towards ITNs. This study identified that the attitude of pregnant women and care takers of children under five years of age to ITNs in this community was fair but upon observation, usage rate was generally very poor in spite of the good knowledge of the benefits of ITNs. Respondents viewed ITNs as a good preventive measure (80%) although less than 48.0% of them who agreed to the fact that it is a good preventive measure used the net. This agrees with Ouattara et al, (2011). 2 % of respondents used MBNS mainly in the rainy season this can be explained by the fact that the bed net provides warmth during the raining season. None of the respondent used the nets during the dry season which is in accordance with Nkessa (2012) who suggests that utilization of ITNs will drop further during the dry season because of increased temperatures. Public health messages need to be intensified for a change of behaviour to increase the regular use of nets. The utilization of mosquito bed nets by the vulnerable populations in Ikwerre LGA was not associated with the knowledge of malaria and awareness of ITNs as a preventive measure against malaria. Other reports have also highlighted the fact that higher levels of education does not necessarily translate to use of appropriate interventions (Njoroge et al 2009). Utilization lagged far behind knowledge. This confirms the studies of Opiyo et al (2007), MNM (2007, 2011), and NMCP (2009). Some of the reasons for not putting the available MBNs into use included: lack of accommodation, lack of space due to number of people in the room, reduction of cooling airflow by ITNs, increased temperatures when using the ITN, lack of proper ventilation, breathing difficulties, skin irritation due to the netting, conflicts with cultural beliefs, the lack of space/resources to use the net, and the inconvenience of tying the net up every day. This reflects similar findings by IRESCO (2011), Astatkie and Feleke, (2007), Dagne et al (2008), and Ayalew et al (2007). These erroneous beliefs need to be dispelled in order to achieve greater levels of utilization. Also a lack of a consistent supply of electricity discouraged some participants to use the net especially during the dry season, as they had no energy source to poor their fans and air-conditions to make their environment cooler for use of the MBNs.
Implications of the Study:
This study identified a poor attitude and practice in use of ITNs among the pregnant women mainly because of lack of awareness. That many residents of Ikwere LGA own ITNs, given to them by the Governments (Federal, State and Local), Non-Governmental Organizations, individuals etc. Despite the level of awareness and the benefits of using ITNs, majority of the respondents could not use them. Attitude towards use is constrained by many factors, ranging from economic, and convenience, religious and cultural influences. Awareness needs to be spread to all community members. This can be achieved through concerted media campaign use of posters and other sensitization method. The federal government of Nigeria will therefore have to improve on provision of social amenities (electricity inclusive) all over the country. Health education in the clinics and infant welfare clinics should promote early and regular use of ITN in pregnancy.
Conclusions:
The level of knowledge on the transmission of malaria and the level of awareness of ITNs as a preventive measure against malaria was high among members in Ikwerre LGA The ownership of MBNs/ITNs among the vulnerable populations of Ikwerre LGA is high (87.2%). Despite the high level of knowledge on the benefit of use of ITNs, attitude towards use was only considered fair. Upon closer study, usage rate seemed lower 12 (8.4%) out of 101 observed nets. The low utilization of ITNs by children below five years old and pregnant women was due not to the lack of ITNs in households The challenges such as lack of accommodations and space, poor airflow and increased temperatures when using the ITN, ITN’s effectiveness, were important personal barriers which affected the respondents attitudes toward the utilization of available MBNs/ITNs.
References:
Abang, J. & Ogoamaka, M.C (1992) Educational Research Methods. Owerri: Totan publishers LTD Nigeria.
Abuja Declaration. (2000). The Abuja Declaration on Roll Back Malaria in Africa by African Heads of States and Governments.
Afolabi BM, Sofola OT, Fatunmbi BS, KomakechW,OkohF,Saliu O, OtsemaborP, Oresanya OB, Amajoh CN, Fasiku D, &Jalingo I(2009). Household possession, use and non-use of treated or untreated mosquito nets in two ecologically diverse regions of Nigeria– Niger Delta and Sahel Savannah.Malaria journal. 8:30
African Union. (2010). Five-year Review of the Abuja call for Accelerated Action Towards Universal Access to HIV/AIDS, Tuberculosis, and Malaria Services by 2010: Progress Report (2006-2010). Accessed at: www.africa-union.org http://ww.who.int/topics/malaria/en/
Astatkie, A. & Feleke, A. (2007). Utilization of Insecticide Treated Nets in Arbaminch Town and the Malarious Villages of ArbaminchZuria District, southern Ethopia.Ethiop. J. Health Dev. 23(3): 206-215.
Amoran, O.E et al (2011). Determinants of Intermittent preventive treatment of malaria during pregnancy(IPTp) utilization in rural towns in western Nigeria Pubmed J. Accessed at :www.ncbi.nlm.nih.gov/m/pubmed/
Baimai, V., Kijchalao, U., et al. (1988). “Geographic distribution and biting behaviour of four species of the Anopheles dirus complex (Diptera: Culicidae) in Thailand.” Southeast Asian J Trop Med Public Health19(1): 151-61.
Binka, . N. &Adongo, P. (1997). Acceptability and use of Insecticide Impregnated bed nets in Northern Ghana. Trop. Med. Int. Health. 2: 499-507
Bishwaranjan P,&Amarendra M. (2009). A review on High burden of malaria during Pregnancy: Need of social science Intervention. Biomed. 3(1):33-38.
Bockarie, M.J. &Dagoro, H. (2006). Are insecticide-treated bednets more protective against Plasmodium falciparum than Plasmodium vivax-infected mosquitoes Abstract)? Malaria Journal 5:15.
Bockarie, M.J, Alexander, N., Bockarie. F., Ibam, E., Barnish, G., &Alpers M. (1996).The late biting habit of parous Anopheles mosquitoes and pre-bedtime exposure of humans to infective female mosquitoes. Trans R Soc Trop Med Hyg. 90(1):23-25.
Cai, X & Deng, D., (1995). “A study on human behavior and socioeconomic factors affecting malaria transmission and control in Qiongzhong, Hainan.” 13(2): 89-93.
Carol A.B, & Celeste M, (2008). Gains in awareness, ownership and use of insecticide treated nets in Nigeria, Senegal, Uganda and Zambia. Malaria Journal.7:153.
CCAM (2009). Malaria and Water Bodies: Strange Bedfellows. Accessed at http://www.cameroon.coalition.org/news/00058.html on 14/08/2011.
CDC, (2010, March). Global health-division of parasitic Diseases and Malaria.Insecticide treated bed nets. Acessed from www.cdc.gov/malaria/.
CDC, (2012, November). Global health-division of parasitic Diseases and Malaria.Anopheles mosquitoes. Acessed from www.cdc.gov/malaria/
Daniel S, ( 2014),P-value calculator for chi-square Test. Accessed from www.danielsopper.com
Dagne, G. &Deressa, W. (2008). Knowledge and Utilization of Insecticide Treated Mosquito Nets Among Freely Supplied Household in WonagoWoreda, Southern Ethiopia. Ethiop. J. Health Dev. 22(1):34-41.
Ehijie F. O. Enato, Augustine O. ;Okhamafe,;Eugen E &Okpere (2007). A survey of knowledge, attitude and practice of malaria management among pregnant women from two health care facilities in Nigeria.ActaObstetricaet Gynecological Scandinavia. 86(1):33-36.
Erhun W, Agbani E, &Adesanya S, (2005). Malaria Prevention : Knowledge, Attitude and Practice in a Southwestern Nigerian Community. African Journal of Biomedical Research.8: 25 – 29.
Federal Ministry of Health.(2005) National Malarial Control Program in Nigeria. Annual Report. Abuja Nigeria.
Federal ministry of health. (2007), National frame work for monitoring and evaluating malaria control in Nigeria. FMOH. Abuja.
Hawley, W. A., Phillips-Howard, P.A., TerKuile, F.O., Terlouw, D.J., Vulule,J. M., Ombok, M., Nahlen, B. L., Gimnig, J. E., Kariuki, S.K., Kolczak, M. S., & Hightower, A. W. (2003). Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in western kenya. American Journal of Tropical Medicine and Hygiene. 68(Suppl4): 121–127, Copyright © 2003 by The American Society of Tropical Medicine and Hygiene
IFRC (2010). Beating malaria with protective nets and community campaigns. Accessed at: http://www.ifrc.org/docs/News/pr10/3010.asp. Retrived 28/04/2011.
IFRC (2010).The Winning Formula to Beat Malaria. Advocacy Report – 2nd edition. Accessed at: http://www.ifrc.org/what/health/diseases/malaria/194500-malaria Report-EN.pdf.
IRESCO (2011). Breaking Barriers: Overcoming erroneous beliefs and practices hindering malaria control in Cameroon
Ikwere LGA (2014) About Ikwerre LGA Accessed at: ikwerrelgaonline.com.ng
Killeen G.F, (2007). Exploring the contributions of bed nets, cattle, insecticides and excitorepellency to malaria control: a deterministic model of mosquito host-seeking behaviour and mortality. Trans R Soc Trop Med Hyg, 101(9):867-880.
Kimbi, K.H., Nyabeyeu, N.H., Ajeagah,U. H., Keka, C.F., Asaah, G.H. & Lehman, L.G. (2010). Overwhelming Malaria Prevalence in Cameroonian School Children. Accessed at http:www.ureddouala.com/download/overwhelming_malariaprevalence_in_cameroonian_schoolchildren.pdf.
Le Goff, G., Robert, V., Fondjo, E. &Carnevale, P. (1992). Efficacy of Insecticide Impregnated Bed Nets to Control Malaria in a Rural Forested Area in Southern Cameroon. Mem. Inst. OswaldoCrutz, Rio de Janeiro.87 (Suppl III): 355-359.
Lin, K., Aung, S., et al. (2000). “Promotion of insecticide-treated mosquito nets in Myanmar.” Southeast Asian J Trop Med Public Health31(3): 444-7.
Malaria Site.(2012) History, Aetiology, Pathophysiology, Clinical Features, Diagnosis, Treatment, Complications And Control Of Malaria. Accessed at http://www.malariasite.com/malaria/AnophelesMosquito.htm.
Maxwell, C.A., Msuya, E., Sudi, M., Njunwa, K.J., Carneiro, I.A., et al. (2002).Effect of community-wide use of insecticide-treated nets for 3–4 years on malaria l morbidity in Tanzania.Tropical Medicine and International Health. 1003–1008.
MNM (2011). “Kenya: Fight against malaria in Shibinga” (2009-2011). Accessed at http://en.malarianomore.nl/werkwijze/projecten/strijd_tegen_malaria__shibinga___west_kenia/.
MNM (2010). “Rectangular Mosquito Nets are a Bad Idea”. Accessed at http://en.Malarianomore.nl/werkwijze/projecten/strijd_tegen_malaria_shibinga_west_kenia/
Ng’ang’a, P. N,Jayasinghe, G.,Kimani, V., Shililu, J.,Kabutha, C., Kabuage, L., John Githure, J.,&Mutero, C. (2008). Bed net use and associated factors in a rice farming community in Central Kenya. Accessed at: http://www.malariajournal.com/content/8/1/64
Njoroge FK, Kimani VN, Ongore D, &Akwale W.S, (2009) Use of insecticide treated bed nets among pregnant women in Kilifi District, Kenya. East Afr Med J.86(7):314- 22).
Nkesa, S.B (2012). Socio-Demographic Factors Influencing the Utilization of Insecticide-Treated Bed Nets Among Vulnerable Groups in the Buea Health District.
Nkuo-Akenji,T., Ntonifor, N. N., Ndukum, M. B., Kimbi, H. K., Abongwa, E. L., Nkwescheu, A., Anong, D. N., Songmbe , M., Boyo, M. G., Ndamukong, K. N., &Titanji, V.P.K. (2006).Environmental factors affecting malaria parasite prevalence in rural Bolifamba, South- West Cameroon. African Journal of Health Sciences.13 (1-2): 40-46.
NMCP (2008).Guidelines For Management of Malaria: Intended for health Personnel. Edition 2008.
NMCP (2009). Report of Activities for 2009 for the Programme for the fight against Malaria
Opiyo, P., Mukabana, W. R., Kiche, I.,Mathenge, E., Killeen, G. F.&Fillinger, U. (2007).An exploratory study of community factors relevant for participatory malaria control on Rusinga Island, western Kenya.Malaria Journal.6( 1) 8.
Ouattara, A. F., Raso, G., Edi, C. V.A., Utzinger, J., Tanner, M., Dagnogo, M. &Koudou, B.G. (2011). Malaria knowledge and long-lasting insecticidal net use in rural communities of central Cote d’Ivoire. Malaria Journal10.
Oresanya, O., Moshe, &Olayemi.T.,(2008). Utilization of insecticide treated bed nets by under-five children in Nigeria: Assessing progress towards Abuja Targets. Malaria Journal accessed at www.malariajournal.com
Park K. (2009). Park’s Text Book of Preventive and Social Medicine. 20thEdition. M/s BanarsidasBhanot, India, p.226.
Tobin West C I, & Alex-Hart B.A (2011). Insecticide-treated bednet ownership and utilization in Rivers State, Nigeria before a state-wide net distribution campaign. J Vector Borne Dis. 48(3):133-137.
Tony,S&Ron,P. (July 2013) Factors that affect the success and failure of Insecticide Treated Net Programs for malaria control in SE Asia and the Western Pacific. Accesdat :www.who.int/malaria/
USAID. (2011). The President’s Malaria Initiative.Fifth Annual Report to Congress.April 2011; p.17. Accessed at :http://www.pmi.gov/resources /reports/pmi_ annual_report11.pdf
Webster, J., Lines J., and Smith, L. (2005). Protecting All Pregnant Women and Children Under Five Years Living in Malaria Endemic Areas in Africa With Insecticide Treated Mosquito Nets.A Working Paper.London School of Hygiene and Tropical Medicine.
WHO (2011). World Health Organization: Annex VII : Procedure for Treating Mosquito Nets and curtains. Accessed at: http://searo.who.int/en/Section10/ Section332/Section554_2554.htm. Acessed 10/07/2011.
WHO. (2010). World Malaria Report 2010. Annex 6, p.176.
WHO.(2000). Water Sanitation and Health (WSH): Water-related Diseases – Malaria. Accessed at :http://www.who.int/water_sanitat ion_health/diseases/ malaria/en/.
WHO: Implementation of the Global Malaria Control Strategy (1993). WHO Technical Report Series, 839 World Health Organization Geneva.
WHOPES . (2005).Guidelines for laboratory and field testing of long lasting insecticidal mosquito nets. Geneva, World Health Organization, 2005 (WHO/CDS/WHOPES/GCDPP/2005.11).












Wonderful and insightful article outlining the need for continuing education and outreach to this huge population at risk. Troubling to see mosquito nets with holes and/or being misused. Also troubling to see less than 50% of pregnant women using netting. It is time to finally mobilize worldwide resources to end this scourge still impacting millions of people which kills up to 500,000 people, mostly children under 5, every year. This is so preventable. Thanks to all the people trying to help. We can make a huge difference through Global Public Health and thanks to all the great people at InfectionControl.tips.
Thank you for such important contributions in Public health sector and especially lives we live everyday!