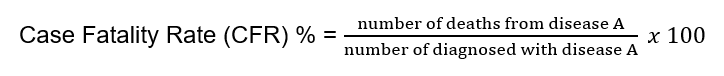
In the science of epidemiology, one term that often comes up is “case fatality rate.” Most of us know that it has something to do with how many people die, but how exactly it is determined and what the difference is with the “mortality rate” is not clearly understood. In simple terms, the fatality rate associated with an infectious disease is the percentage of people who die from a particular disease in relation to all the people who have been diagnosed with that disease. For example, if 10 people have died out of 100 who were diagnosed with the same disease, the fatality rate is 10%.
Now, one of the things to understand is that the CFR has certain dependencies. The CFR can vary significantly based on the location and condition of the population, and they can vary over time. The latter will become very important once treatment or preventive options like vaccines become available. The former might indicate any underlying health concerns, population age, initial treatment options etc.
For example, for COVID-19, global case fatalities ranged 1.7%–39.0% in February to March of 2020 and fell below 0.3% in July to August 2022 (Horita N., Fukumoto T, 2023). The bottom line is that the CFR for certain diseases is generally not a fixed number and will change over time. However, having said that, according to the WHO (2023) Rabies has a fatality rate of almost 100 % once clinical symptoms appear. That is very scary. However, the good news is that an effective post-exposure prophylactic treatment is available. For Ebola, the CFR can vary from 25 to 90%.
Another thing to remember is that the CFR counts those who have been diagnosed with the disease. To do that, public health officials have to know that you have the disease, which happens most of the time only if you get tested, and there is a record of being diagnosed. As we have seen with COVID, those who had severe symptoms were seen by health professionals, and many with minor or no symptoms did not get tested. In other words, the total number of individuals having the disease is often much higher. Consequently, the fatality rate is lower.
mortality rate
As previously mentioned, another term often used is “mortality rate.” The mortality rate is calculated by taking the number of deaths (e.g., disease A) per number of individuals in a given population. So, the “denominator” in our equation is now independent of being diagnosed, sick, or not. It’s based on the total population within a given geographical area, like city, or country. It can be calculated for every 1000, or 100,000 and has a timeframe associated with it, for example, per year. One of the shortcomings, and the same with the CFR, is that the counted deaths need to be associated with the disease in question. Early in the COVID pandemic, Europe registered around 98% of the COVID deaths, while in African regions, that was only 10% (WHO). Another factor that makes these assessments more difficult is the difference in what is considered a “COVID” death. In many cases but not all, it is based on COVID being the underlying or contributing factor.
WHO (2022) reported that 3 million excess deaths worldwide were associated with the COVID-19 pandemic in 2020 and 2021. The term “excess” death is used to describe deaths outside of normal mortality for a given population and time frame.
As of March 20, 2024, there were 704 million cases of COVID-19 and 7 million deaths, as posted by the “Worldometer” (2024). Any attempt to calculate the true CFR with these numbers is prone to failure, as discussed above. Now, case in point, one case study performed in New York (2020), showed that actual cases were 10x higher than the number of confirmed cases, and the actual deaths were almost twice the number of confirmed deaths which led to a CFR of 1.4% at that time. The mortality rate was calculated to be 0.28% based on the population of New York at that time.
So, where does that leave us with the use of these terms and their underlying data? In general, both terms have value and provide useful insight into the severity and mortality of an infectious disease. Knowing their limitations based on the data sets used is important for public health decision-making, including prioritization of resources, research emphasis, and overall response.
References
Horita N., Fukumoto T., (2023). Global case fatality rate from COVID-19 has decreased by 96.8% during 2.5 years of the pandemic. J. Med. Virol., 95 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9874414/
WHO (2023) Rabies key facts. https://www.who.int/news-room/fact-sheets/detail/rabies#:~:text=Overview,rabies%20is%20virtually%20100%25%20fatal.
WHO (2022). The true death toll of COVID-19: estimating global excess mortality. https://www.who.int/data/stories/the-true-death-toll-of-covid-19-estimating-global-excess-mortality
Worldometers (2024). COVID-19 CORONAVIRUS PANDEMIC, https://www.worldometers.info/coronavirus/
New York State (2020). Amid Ongoing COVID-19 Pandemic, Governor Cuomo Announces Results of Completed Antibody Testing Study of 15,000 People Showing 12.3 Percent of Population Has COVID-19 Antibodies. https://www.governor.ny.gov/news/amid-ongoing-covid-19-pandemic-governor-cuomo-announces-results-completed-antibody-testing