Abstract:
The misuse of antibiotics coupled to a decrease in the number of novel drugs entering the clinic has led to the development of antibiotic resistant bacteria. To prevent this from happening, antibiotics should only be taken when necessary and if taken, the entire prescription should be consumed.
Main Article:
You feel the onset of a cold coming on and decide to head to the doctor for a checkup. As a safety precaution, the doctor prescribes you an antibiotic and tells you to begin taking it if your symptoms worsen. In the case that you do become more ill, the antibiotics are a great resource to help clear up a bacterial infection, an option that many people did not have before the discovery of antibiotics in the late 1920’s. However, it must be noted that with great power comes great responsibility.
Alexander Fleming discovered penicillin in 1928, which launched a cascade of discovery of novel antibiotics in the coming years. This was arguably the most important discovery that has led to an increase in the quality of life and life expectancy of humans. With the many new antimicrobial drugs being found, it was easy to visit the doctor when you became sick because the prescribed antibiotics worked effectively and you were back to feeling great in a relatively short amount of time.
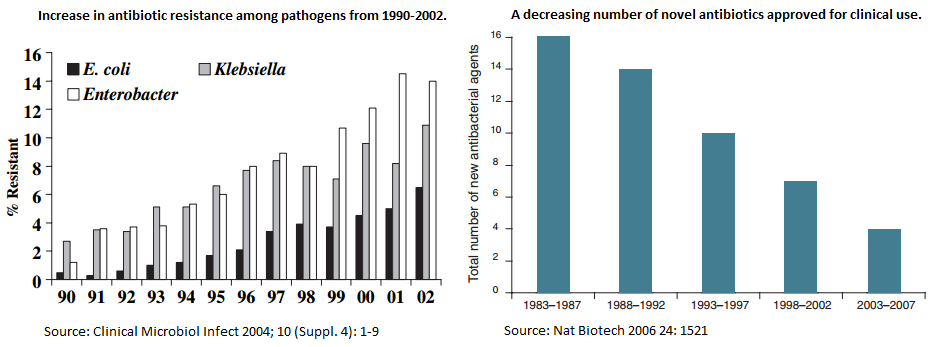
In recent years, antibiotics have become less effective and the increase in antibiotic resistance has skyrocketed. It is also important to note that the amount of novel antibiotics being discovered is decreasing (Figure 1). This poses a new danger where antibiotics that have previously wiped out infections are now struggling to combat waves of resistant bacteria.
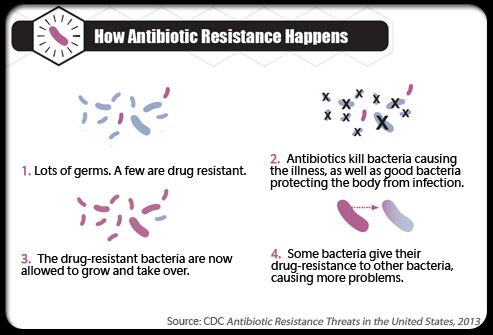
Some of the reasons for this increase in resistance are the misuse of antibiotics and the tendency for them to be overprescribed. In order to understand why, let’s take a look at one way which antibiotic resistance becomes prevalent. When a bacterial culture is growing in a host organism, each bacterium is slightly different from the one next to it in terms of their genetic code. Because of this, some bacteria may have alterations in their DNA that will allow them to become resistant to an antibiotic. Upon the introduction of an antibiotic, such as one prescribed by a doctor, many of the non-resistant bacteria will be eradicated, but the few resistant bacteria will remain. At this point, the bacterial population is greatly diminished allowing the immune system to overpower the infection and clear it from the host.
In another case where the patient uses the antibiotics incorrectly, there is a greater risk for the generation of antibiotic resistant bacteria that has the potential to become a serious clinical issue. When prescribed an antibiotic, it is extremely important to take the full dose for as long as the doctor prescribed and not to discontinue use in the event that symptoms improve. Interrupting the antibiotic dosage prematurely can accelerate the rebound of resistant bacteria. The drug has a shorter duration to accomplish the job, leaving a larger population of unharmed and resistant bacteria that are able to multiply, causing the patient to become sick with a population of resistant bacteria. In this event, it will be much more difficult for the host’s immune system to combat the infection and other drug therapies may be required (Figure 2).
The take home message is to take great care to prevent the misuse of antibiotics. Once prescribed, they should only be used if absolutely necessary, such as when symptoms worsen significantly. Antibiotics should not be taken if you are feeling under the weather and wish to accelerate the recovery. Give your immune system a chance to take over the infection and strengthen your immunity for the future in the occasion that you are infected by the same organism.
References:
- Livermore, D. M. The need for new antibiotics. Clinical Microbiol Infect. 2004, (Suppl. 4), 1-9.
- Fox, J. L. The business of developing antibacterials. Nature Biotechnology. 2006, 24(12), 1521-1528.
- Antibiotic Resistance Threats in the United States, 2013.













[…] https://infectioncontrol.tips/2015/11/13/importance-of-using-antibiotics-correctly-and-completing-th… […]