Abstract:
Patients are especially prone to infections of the bloodstream when they are receiving medicines and nutrients through central and peripheral lines. At the Infection Prevention and Control Conference (Knowlex), held in London on February 23, 2016, Corinne Cameron-Watson, a senior infection prevention and control nurse, presented the findings from a study in the UK monitoring the use of port cleaning devices to reduce catheter-related bacteremia. The use of the system greatly improved staff compliance to cleaning practices, while reducing bloodstream infections in a pilot 6-month study.
Main Article:
Bloodstream infections (BSI) are a prevalent issue in hospitals worldwide, but were occurring at a slighter higher rate at the Barking, Havering and Redbridge University Hospitals (UK)1. Typically, pathogens enter the bloodstream through intravenous tubes, or central line catheters2. These catheters are essential for many patients, but are prone to contamination with multiple types of pathogens. This is of great concern, as the typical barriers to infection (skin, mucosal layers) are completely bypassed when a central line is used. Once in the blood stream, the pathogens can easily multiply and propagate throughout the body1. Thus, prevention is the especially emphasized in BSI management.
Injection of medicines through the central line is performed using ports connected to the intravenous system. Typical protocols require scrubbing of the ports for a minimum of 15 seconds, followed by a minimum of 30 seconds drying time. The CurosTM system (Vygon Ltd) is a small piece of equipment that is used to provide a constant, clean barrier to the line. The port protector is placed over the port, and passively cleans the port using 70% isopropanol within three minutes3. One benefit of the Curos system is that complacency from staff is avoided completely using this system.
This system abides to the of Aseptic Non Touch Technique (ANTT) for reducing infections, but does not strictly adhere to Epic3, a series of guidelines for reducing healthcare acquired infections (HAI’s), which recommend disinfection with alcohol swabs directly4.
Study:
The study was performed in four separate hospitals wards, where intravascular lines are regularly used. To establish a baseline, BSI date was gathered for 6 months prior to the trial. Monthly audits were performed during the trial.
In a staff survey disseminated to the study it was revealed that the hospitals involved in the study were well below the national average for adherence to the outlined guidelines for port decontamination. Cleaning of the port relied on three main factors:
1) Proper technique while cleaning (scrubbing or twisting action is required);
2) Duration of the physical cleaning (minimum 15 seconds); and
3) Duration of the disinfectant drying/kill time (minimum 30 seconds).
The national average shows that 46% of respondents only cleaned for 10 seconds or less. This is an improvement compared to the Barking, Havering and Redbridge (BHR) University Hospitals, where 54% of respondents cleaned for 10 seconds or less. Similarly, the national average of respondents that dried for 25 seconds or less was 57%, whereas the BHR hospitals average was 75%. From this data, it is evident that BHR university hospitals’ compliance to the guidelines were well below the national average.
Following appropriate training, the use of Curos was evaluated for 6 months. Four wards, including oncology, acute care for the elderly, adult intensive care, and the surgical wards, were monitored monthly at two different hospital sites. BSI rates, as well as user questionnaires were obtained to determine satisfaction with the system.
Although no data was available for compliance to cleaning of IV ports prior to the study, based on survey responses, compliance was estimated to be approximately 27%. Using the Curos system, compliance was increased to 80% (on average across four different sites) in 6 months alone (Figure 1).
Figure 1- Comparison of Compliance Vs Incidence of Line Related Bacteremia
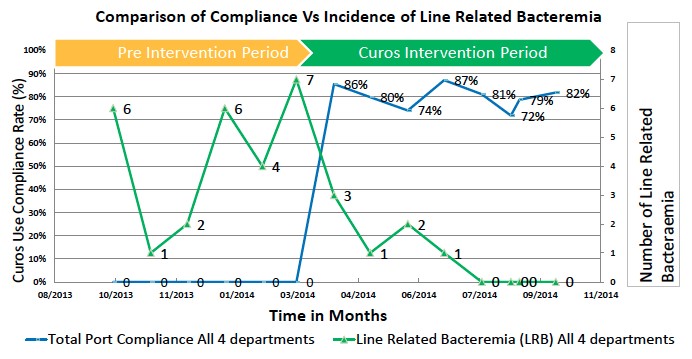
Catheter related blood stream infection (CRBSI) rates were monitored for 6 months prior to implementation of the Curos system. In this period, the hospitals experienced 26 different instances of CRBSI, and this cost £161,434 to treat peripheral line infections, and £416,000 to treat central line infections (Figure 1). Following implementation of Curos, the hospitals only had 4 CRBSI’s (three of which occurred in the first month). From a financial standpoint, this cost the NIH a total of £24,836 to treat peripheral line infections, and £64,000 to treat central line infections. This is a reduction of over 69%!
The cost of implementing the Curos system costs each ward approximately £6,857.24 for each hospital. Split among each of the four wards, this cost would be approximately equivalent to the cost of treating one patient for CRBSI per year. Accounting for the cost of products, the four hospitals saved approximately £130,400 from peripheral line infections and £345,802.11 from central line infections.
Survey results from both patients and staff were highly favourable. Staff found the system easy to use, more convenient, and most importantly, more effective than the old method. Patient surveys revealed that they appreciated the visibility of the system, providing additional reassurance of their safety while in the hospital.
Conclusion:
The current practices to reduce catheter-related bloodstream infections are effective for preventing contamination, but low compliance greatly hinders its benefits. The use of a novel system, such as the Curos system, was shown to be effective in reducing CRBSI’s and the costs associated with its treatment. Implementation of simple devices such as this system can yield much greater benefits by addressing the unfortunate, but very pervasive issue of compliance.
Video: https://www.youtube.com/watch?v=0Flt1esoz_c&index=14&list=PLXw6r9VD6y_5IG6TJ9_Jv8vmNTyu901x8
Sides: https://media.wix.com/ugd/f70a7d_b4bb5576672a476bb1c4bba0a873dd07.pdf
About Knowlex:
Knowlex, shorthand for ‘Knowledge Exchange’, is a new organisation that has been set up with the ambition of disseminating information on research and innovative practice to help healthcare professionals in their working lives.
Upcoming Conference:
Tuesday 6th September 2016 RNCM Manchester, UK
European City of Science 2016
In light of estimates that the total cost of AMR to healthcare systems within OECD countries will reach £1.9 trillion by 2050, on 8th September 2016, Knowlex will welcome more than 350 healthcare professionals to Manchester, European City of Science, for Infection Prevention & control 2016.
Conference Website: http://www.infectioncontrolmanchester2016.co.uk/
References:
- Center for Disease Control (2016) Central Line-associated Bloodstream Infection (CLABSI). Center for Disease Control. Accessed June 17, 2016 http://www.cdc.gov/hai/bsi/bsi.html
- Klompas M, Branson R, Eichenwald EC, Greene LR, Howell MD, Lee G et al (2014) Strategies to Prevent Ventilator-Associated Pneumonia in Acute Care Hospitals: 2014 Update. Infection Control & Hospital Epidemiology 35, 133-154
- Vygon UK, Ltd (2016) Curos Disinfecting Port Protectors. Accessed June 17, 2016. http://disinfectingcap.co.uk/?utm_source=Vygon&utm_medium=News&utm_campaign=News-Vygon
- Loveday, H. P., Wilson, J., Pratt, R. J., Golsorkhi, M., Tingle, A., Bak, A., … & Wilcox, M. (2014). epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection, 86, S1-S70.











