Abstract:
In this article, an introductory overview of managing the Infection risks during a disaster or mass casualty event is presented. Reaching an understanding of the key terms and definitions and then expanding on the basic overview of setting up a Infection Preventionist program.
Main Article:
Introduction
In disaster situations, using standard protocols are not sufficient. In this article, a general overview of the key areas to consider when faced with a disaster will be presented, as well as key terminology. It is very difficult to inform general policies on how to manage specific diseases or patients. Instead, a guide on how to draft personalized hospital, site or regional specific plans will be presented. Every hospital/region will have its own plans and regular exercises need to be held (desk-top or field), whether in-hospital or pre-hospital.
Definitions:
Disaster:
Often thought of as natural events; earthquakes, tornados, tsunami’s etc.
(Major) Incident:
Man made events; acts of terror, train/bus crashes, stadium incidents etc.
Disaster Management:
A disaster can be said to have occurred; When normal community/regional resources are overwhelmed, or are in adequate. This event then calls for an extraordinary response. (1)
Disaster Medicine:
The combination of medical and organizational measures undertaken in case of a disaster/incident covering the entire range of medical care from the scene of the disaster to the hospital bed.
Most disaster/major incident programs follow various phases of response frameworks. In this report, a framework employed in South Africa will be presented.
The Disaster Management Act of South Africa (No.57 of 2002) describes the following phases of a disaster: (2)
- Pre-Disaster Risk Reduction:
- Prevention
- Mitigation
- Preparedness
- Early Warning
- Post-Disaster Risk Reduction:
- Response
- Recovery
- Rehabilitation
- Reconstruction
Disaster medicine is neither clean nor pretty. Work is done under intense pressure, and getting your hands dirty is par for the course. The ability to triage brings it own stresses. Recovery work can last days or weeks, and sleep deprivation becomes a reality, which further adds to the risk of managing infections.
Infections, unsanitary working and living conditions, are of concern in a “normal” environment, and are exacerbated in a disaster scenario, for both healthcare workers and the local populations. Sound pre-planning, established protocols and procedures, are vital for the health and welfare of all concerned. This will aid healthcare workers in containing the potential spread of disease and improve the living conditions for those affected.
Methods of the interventions
It starts with and ends with personal hygiene, and your ability to prevent body substance contamination.
It is critical in a disaster setting that a person is assigned the role of an Infection Prevention Control Officer, or Infection Preventionist (IP). The primary function of this trained person is to be fully extremely familiar with ALL infection prevention principles and practices that need to be implemented in a disaster scenario. The IP should further ensure that the standards are met and maintained during all phases of the disaster process. Depending on the duration of the disaster/medical outbreak (as in the ongoing West Africa Ebola outbreak), local persons should be trained and sent out into the field to work with remote teams to coordinate the remote field IP work. Local health care facilities and public health officials must be incorporated into the planning phase as they will be aware of additional local/regional resources which may be in a position to assist.
Outcomes
Successful outcomes, post disaster, is heavily reliant on the ability to plan and thoroughly prepare. Hence a sound preparedness strategy is the foundation of minimising the incidences of infection during and post event.
The Infection Chain – We need to break the chain, that is the task of your IP (3)
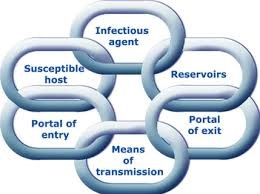
Areas of importance with respect to managing and minimising infections during disasters would be the following:
- Personal Protection Protocols and Equipment
- Prophylaxis protocols and the necessary drugs to treat the healthcare workers
- Trend analysis of recent global disaster (and in todays political climate) acts of terror
- Routes of Contamination/Infection
- Weather/climate (hinder or aid)
- Management of the environment, how it could aid or harm your IP’s efforts
- Management of medical equipment, patient transportation vehicles.
Ongoing education is key to the success of reducing the incidence of infection during a disaster. The groundwork for this success will be laid long before teams are sent to sites. The following table outlines education topics that IP’s need to cover when developing training
materials for staff, patients, and visitors. These materials should be drafted and updated on an ongoing basis, in readiness to be used when on deployment.
Education topics requiring Infection Preventionist (IP) involvement |
|
Education topics IP’s need to cover for staff, patients, and visitors |
| Patient decontamination |
| Patient management (patient discharge instructions, when to isolate, and others) |
| Disease-specific information on bioterrorism agents, emerging infections & pandemic influenza |
| Self-screening and reporting of symptoms |
| Isolation procedures |
| PPE use and reuse |
| Procedures for obtaining and handling patient specimens safely |
| Hand hygiene |
| Respiratory etiquette |
| Cleaning and disinfection of toys in shelters |
| Cot or sleeping area configuration for evacuation shelters |
| Waste management |
| Emergency management procedures and policies that affect infection transmission |
| How to safely reuse respiratory protection when resources are insufficient or unavailable |
| Postmortem care |
Table Courtesy of American Journal of Infection Control – May 2009 (4)
During response to a mass casualty incident, all responding staff will require some level of training that is specific to the event. IPs should have ‘‘just in time’’ training materials on hand (covering all the relevant trending disaster/mass casualty events), so that they can distribute them during the disaster response, and use them as toolbox talk topics during shift change overs on-site or in the field.
Conclusion
Key to managing infection control at a disaster/mass casualty event is to have a well trained IP team, with sound leadership and fully conversant of the challenges to be faced. A good IP will be an integral part of your medical and ERT rapid response teams, if not one of the team, cross trained as an IP Practitioner.
References:
- Disaster Medicine, MMED Univ UCT & Stellenbosch, course notes, Chap 1
- The Disaster Management Act of SA (No.57 of 2002: Disaster Management Act 2002)
- http://study.com/academy/lesson/chain-of-infection-definition-example.html
- Table Courtesy of American Journal of Infection Control, May 2009, Vol 37 http://dx.doi.org/10.1016/j.ajic.2008.12.002
Additional Reading:
http://www.who.int/gpsc/5may/Glove_Use_Information_Leaflet.pdf












