Abstract
Hand hygiene is the best method to prevent the transmission of infections. Hand hygiene for hospitalized patients sounds obvious – something that should be easy to accomplish and regarded as important to the patient experience. However, patient hand hygiene is a problem for most hospitals today. It is difficult to accomplish and not monitored by healthcare personnel. No infection preventionist will argue against the importance of patient hand hygiene. However, since it is neither prioritized nor measured by hospitals, it falls through the cracks. This, coupled with the fact that more and more research points to patients as the “missing link” in infection control efforts means that, in order to reduce hospital acquired infections (HAIs), hospitals need dedicated efforts to improve patient hand hygiene. Key to achieving these efforts is empowering patients to make hand hygiene easy to do on their own and to understand the critical importance cleaning their hands plays in preventative care.
Main Article
Background and Introduction
You are a patient in a hospital bed. Like many patients you fear getting an infection while hospitalized. Your hands need cleaning, but you do not have the resources within easy reach – both the sink and the wall mounted hand sanitizer dispenser are too far away. You could use the nurse call button for assistance, but are reluctant because you do not wish to be bothersome to your caregivers – you know how busy the hospital staff is. Yet, just waiting for a staff member to come to your room to help is stressful. How can we improve this scenario? Cleaning your hands sounds very simple but for hospital patients, the scenario described is too often the norm in terms of their patient experience.
Hand hygiene, our most effective means to prevent infection transmission, is elusive to many hospitalized patients. Most of us will be a patient in our lifetime or have a loved one hospitalized. Empowering patients to perform hand hygiene is crucial.
Recognizing the Problem
No one argues against patient hand hygiene but very few are engaged in empowering patients to perform hand hygiene. The need for greater focus on patient hand hygiene was identified in a study that stated that patient hand hygiene may prove critical to the prevention of hospital acquired infections (HAIs) (Landers, 2012). When it comes to hand hygiene, healthcare has traditionally focused on healthcare workers (HCWs) with little to scant attention to patients and visitors. However, this study helped bring the issue of patient hand hygiene to the forefront of infection control efforts:
“To date, initiatives aimed at improving hand hygiene have primarily targeted HCW practices, without full consideration of the patient and the patient’s caregiver network. However, emerging evidence suggests that most infections occur as a result of bacteria present within the patient’s own flora and bacteria present on surfaces within the health care environment. Because patients and HCWs touch surrounding items and surfaces, including patients in the performance of hand hygiene could decrease pathogen transmission and the risk of health care–associated infections.” (Landers, 2012).
As noted above, patients frequently fear getting an infection when admitted to the hospital and approximately 1 in 25 (CDC, 2016) patients suffer from a HAI. This is a realistic fear and one that the healthcare industry should be trying to address with all means available. Patient hand hygiene should be an essential part of every healthcare provider’s infection control program.
Hand hygiene is a simple skill, but accomplishing it at every appropriate opportunity within the healthcare environment is complex. A disconnect between nurses’ and patients’ perceptions of the frequency of patients being provided opportunities for hand hygiene was demonstrated in which 64% of nurses reported offering hand hygiene to patients while only 14% of patients agreed with that (Burnett , 2008). Awareness of the importance of patient hand hygiene and proactive attitudes toward this task have life and death consequences. Patients can easily be empowered to perform their own hand hygiene in many instances.
Addressing Patient Hand Hygiene
Interventions can be effective. A recent study demonstrated a reduction in Clostridium difficile infections when patients were given an educational program along with opportunities to perform hand hygiene (Pokrywka, 2017). C. difficile infection events decreased significantly (p ≤ 0.05) for 6 months after the interventions were implemented. In addition, another study demonstrated the need for a patient centric approach to hand hygiene (Rai, 2017). This study detailed five moments for patient hand hygiene mirroring the World Health Organization (WHO) format of the five moments of hand hygiene for healthcare personnel. Patient hand hygiene resulted in reduced infections or colonization of bacterial pathogens and respiratory viruses.
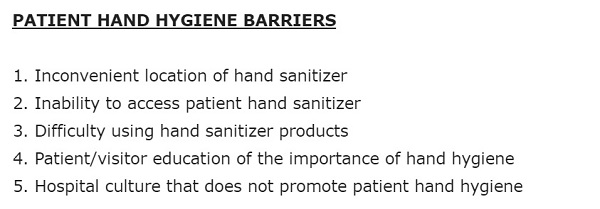
Education has a major role in patient and visitor hand hygiene. Many studies have stated the necessity of educating staff, patients, and visitors to improve consistent hand hygiene (Cheng 2016, Vaidotas, 2015, Willison-Parry, 2013, and Ardizzone, 2012). Removing barriers to performing hand hygiene, such as the inconvenient location of hand sanitizer (Hobbs, 2016 and Cure, 2015) – what most regard as the primary barrier – or difficult to use hand sanitizer products, are also critical to the success of a patient hand hygiene program (Figure 1) (O’Connell, 2015 and Knighton, 2017).
Figure 1: Issues resulting in hand hygiene barriers
The details of incorporating patient hand hygiene into infection control policy are best explored and met by bedside staff. Change in workplace behavior takes consistent effort. Healthcare culture also impacts the performance of patient hand hygiene. It was stated in a recent article that:
“Most executives, regardless of industry, will agree that culture eats strategy for lunch. Despite the best planning and implementation of patient safety interventions in hospitals, quality improvement initiatives frequently fail or fall short of internal targets. Organizational resistance to change is a well understood phenomenon, but one that is poorly applied to healthcare.” (Wallace, 2016)
Antibiotic Resistance
On the global issue of antibiotic resistance, the prevention of infections takes on major importance. HAIs are a major cause of morbidity and mortality. Bacteria cause HAIs and 70% of these bacteria are resistant to one of the drugs used to treat them (Spellberg, 2009). Many studies have demonstrated the presence of pathogenic organisms on the hands of patients. After only 48 hours of hospitalization, 39% of tested patients had at least one pathogenic organism and 8% were contaminated with two or more pathogens (Istenes, 2013 and 2011). This issue should be a powerful force for culture change in healthcare. Without antibiotics, infection prevention is imperative and patient hand hygiene is going to become more critical to infection prevention efforts.
Costs
Hospitals in the US can spend as much as 10% of their operating budget on infection control. Patients with infections stay an average of 19 days longer in the hospital (Lucado, 2010). In addition, HAIs costs continue long after the patient is discharged with extra follow-up visits and prescription costs (Wallace, 2016). Longer recovery times impact society as a whole with the disruption of family and work life. Since most infections are preventable, simply put, these costs are unnecessary.
Conclusion and Significance
Infections are destructive and require vigilance to address. Empowering patients with the ability to clean their hands without the help of a caregiver is a major step towards preventing HAIs. The issue of patient hand hygiene has been ignored for too long; patients need awareness and resources.
Empowering patients deserves a forceful commitment from all management and staff. We have the knowledge but we need attitudes and culture to internalize the importance of empowering patients. Patient hand hygiene is lifesaving. We ignore it at our own peril.
References
Ardizzone, L., Smolowitz, J., Kline, N., Thom, B., and Larson, E. (2013). Patient hand hygiene practices in surgical patients. American Journal of Infection Control, 41(6), 487-491.
Burnett, E., Lee, K. and Kydd, P. (2008). Hand hygiene: What about our patients? Journal of Infection Prevention, 9 (1), 19-24.
Center for Disease Control: http://www..cdc.gov/features/handwashing/.
Cheng, V., Tai, J., Li, W., Chau, S., Wong, L., Ching, R., Ng, M., Ho, S., Lee, D., Lee, W., Wong, S., and Yuen, K. (2016). Implementation of directly observed patient hand hygiene for hospitalized patients by hand hygiene ambassadors in Hong Kong. American Journal of Infection Control. 44(6), 621-624.
Cure, L., and Van Enk, R. (2015). Effect of hand sanitizer location on hand hygiene compliance. American Journal of Infection Control, 43(9), 917-921.
Hobbs, M., Robinson, S., Neyens, D., and Steed C. (2016). Visitor characteristics and alcohol-based hand sanitizer dispenser locations at the hospital entrance: Effect on visitor use rates. American Journal of Infection Control, 44(3), 258-262.
Istenes, N., Bingham, J., Hazelett, S., Fleming, E., and Kirk, J. (2013). Patients’ potential role in the transmission of health care-associated infections: Prevalence of contamination with bacterial pathogens and patient attitudes toward hand hygiene. American Journal of Infection Control, 41(9), 793-798.
Istenes, N., Hazelett, S., Bingham, J., Kirk, J., Abell, G., and Fleming, E. (2011). Hand hygiene in healthcare: The role of the patient. American Journal of Infection Control, 39(5), E182.
Knighton, S., McDowell, C., Rai, H., Higgins, P., Burant, C., and Donskey, C. (2017). Feasibility: An important but neglected issue in patient hand hygiene. American Journal of Infection Control, 45(6), 626-629.
Landers, T., Abusalem, S, Coty, M., and Bingham, J. (2012). Patient-centered hand hygiene: The next step in infection prevention. American Journal of Infection Control, 40(4), S11-S17.
Lucado, J., Paez, K., Andrews, R. and Steiner, C. (2010). Adult hospital stays with infections due to medical care, 2007, Agency for Healthcare Research and Quality, Statistical Brief #94.
Pokrywka, M., Buraczewski, M., Frank, D., Dixon H., Ferrelli, J., Shutt, K., and Yassin, M. (2017). Can improving patient hand hygiene impact Clostridium difficile infection events at an academic medical center? American Journal of Infection Control, 45(9), 959-963.
Rai, H., Knighton, S., Zabarsky, T., and Donskey, C (2017). A randomized trial to determine the impact of a 5 moments for patient hand hygiene educational intervention on patient hand hygiene. American Journal of Infection Control, 45(5), 551-553.
Spellberg, B. (2009). Rising plague: The global threat from deadly bacteria and our dwindling arsenal to fight them. Amherst, N.Y. : Prometheus Books
Vaidotas, M., Kiyomi, P., Yokota, O. Marra, A., Zinsly, T. Camargo, S., Victor, E., Gysi, D., Leal, F., Santos, F., and Edmond, M. (2015). Measuring hand hygiene compliance rates at hospital entrances. American Journal of Infection Control, 43(7), 694-696.
Wallace, N., Cropp, B., and Coles, J. (2016). Insurance companies pay the price for HAIs. Retrieved from https://infectioncontrol.tips/2016/06/15/insurance-companies-pat-the-price-for-hais/
Willison-Parry, T., Haidar, E., Martini, L., and Coates, A. (2013). Handwashing adherence by visitors is poor: Is there a simple solution? American Journal of Infection Control, 41(10), 928-929.












