Peer Reviewed
Abstract
Background: Hand hygiene is the most effective measure to prevent healthcare-associated infections. However, the role of residents’ hand hygiene is unexplored.
Purpose: To test the feasibility and acceptability of a resident-focused hand hygiene intervention within a long-term care facility.
Methods
The qualitative phase began with direct observation, followed by interviews of six residents and six staff members using a semi-structured interview guide.. The study included four researcher-developed tools for use in the quantitative phase: 1) Flowsheet for Hand Hygiene Observation, 2) The Participant Demographics and Environmental Context Questionnaire, 3) Risk for Healthcare-Associated Infections Tool, and 4) Health Beliefs Related to Hand Hygiene Tool. In addition, the researcher recorded the participant’s reaction to the hand hygiene intervention using a modified Participant’s Reaction to the Hand Hygiene Intervention questionnaire, derived from the World Health Organization’s (2009) Perception of Hand Hygiene Survey.
Significance/Results
While hand hygiene opportunities were constant for all participants eating in the dining hall, respiratory hygiene opportunities and episodes of T-zone touching varied. Although hand hygiene increased minimally, the mean percentage of adherence to respiratory hygiene increased, with a decrease in the range of T-zone touching following the intervention. These findings suggest the participants were more aware of the role of respiratory hygiene and T-zone touching in disease transmission after the intervention. There were medium or large effect sizes noted in all sub-scales of the Health Beliefs Related to Hand Hygiene Tool. Measures of central tendency described the total scale and item-level means on the Participant’s Reaction to Hand Hygiene Intervention questionnaire. Findings suggest the residents tolerated the wipes and valued the educational intervention.
Conclusion
This feasibility study assessed current hand hygiene behaviors in the long-term care facility residents. The study incorporated behavior modification and hand hygiene research to inform future studies to establish evidence-based practice to prevent healthcare-associated infections. The intervention may enhance self-efficacy as the skill remains with the resident regardless of setting or staffing. In addition, the study provided initial psychometric evidence for the researcher developed tools and provided key information to direct future development of the tools.
Introduction
In the United States, approximately three million people in all healthcare settings develop healthcare-associated infections annually (Centers for Disease Control [CDC], 2016; Office of Disease Prevention and Health Promotion [ODHP], 2013). Hand hygiene is a strategy to prevent infections because hands are the most common vehicle of disease transmission. Adherence to hand hygiene continues to be suboptimal in all settings, despite evidence indicating providers understand the significance of hand hygiene (World Health Organization [WHO], 2009). Therefore, hand hygiene has been deemed a quality indicator, with mandated public disclosure (WHO, 2009).
Given the prevalence and impact of infections, research and prevention have historically focused on providers’ adherence to hand hygiene, leaving the effect of residents’ hand hygiene largely unexplored. Studies have validated the importance of hospital patient hand hygiene, suggesting patients’ hands become a reservoir and a means of transmission when hands are not adequately cleansed (Burnett, Lee, & Kydd, 2008; Lawrence, 1983).
As many long-term care facilities lack specialized infection control staff, infection control and surveillance can be challenging in this setting. Long-term care facilities serve populations with diminished immune response or malnutrition, which increases the risk of infections. Long-term care residents may also have multiple co-morbidities or polypharmacy, which can further compromise the immune system (Smith et al., 2008). Cognitive or functional ability of residents may increase their need for hand hygiene while decreasing their ability to perform it. In long-term care facilities, two major factors increase risk of transmission through direct or indirect contact: 1) Medicaid reimburses for semi-private rooms and 2) long-term care facilities promote socialization of residents. As a result, residents are susceptible to transmission and subsequent colonization with infectious organisms.
The conceptual framework for the study was the Health Belief Model (Figure 1). Four psychologists developed this social cognitive model in the 1950s to examine barriers to preventive health programs (Rosenstock, 1974). The Health Belief Model has been widely used to understand differing behaviors or attitudes under the same condition and has been previously tested as a theoretical model to measure healthcare providers’ attitudes toward hand hygiene (Kretzer & Larson, 1998). The Health Belief Model allowed the researcher to identify and understand barriers to resident hand hygiene, thus making it a good fit for a feasibility study.
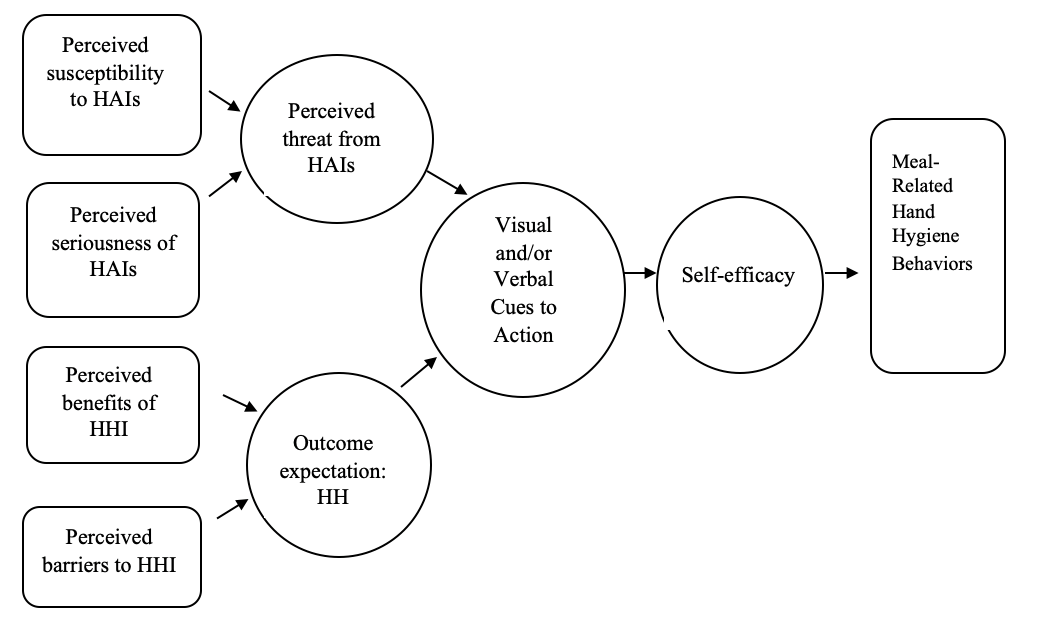
Figure 1: Health Belief Model Applied to Resident-Focused Hand Hygiene
Note: HAIs = Healthcare-Associated Infections; HHI = Hand Hygiene Intervention; HH = Hand Hygiene
The original model had four constructs: perceived susceptibility, perceived seriousness, perceived benefit, and perceived barriers to action (Rosenstock, 1990). Two additional constructs were later added: cues to action and self-efficacy (Rosenstock, 1990). According to the theory, for an individual to take preventive action, such as hand hygiene, the individual must first perceive he/she is personally susceptible to a health risk, such as a healthcare-associated infection. Next, the health risk (infections) must have at least a moderately serious impact on some component of the individual’s life. Furthermore, the advised preventive health action must be beneficial, reducing the individual’s susceptibility to the health risk or the seriousness of the health risk. Lastly, taking the advised preventive health action must not exceed tangible and/or psychological costs (Rosenstock, 1974). In other words, when an individual believes a health risk can be avoided, has a positive expectation that taking a recommended action will lead to avoiding the health risk, and believes he/she can successfully complete the advised preventive health action, the individual is more likely to complete the advised preventive health action.
The purpose of this study was to test the feasibility and acceptability of a resident-focused hand hygiene intervention within a long-term care facility using the World Health Organization’s Participant’s Reaction to the Hand Hygiene Intervention Questionnaire (WHO, 2009). Although this tool is established and widely accepted, there was no reported reliability or validity data found in the literature. The World Health Organization’s original questionnaire was modified for use in the study.
Methods
The study followed an exploratory sequential mixed methods design. Phases were implemented sequentially, starting with qualitative data collection and analysis. Detailed study procedures for the qualitative phase (Figure 2) included researcher observation of all meals in dining hall on one weekday and one weekend day in the setting for feasibility issues and to identify barriers.
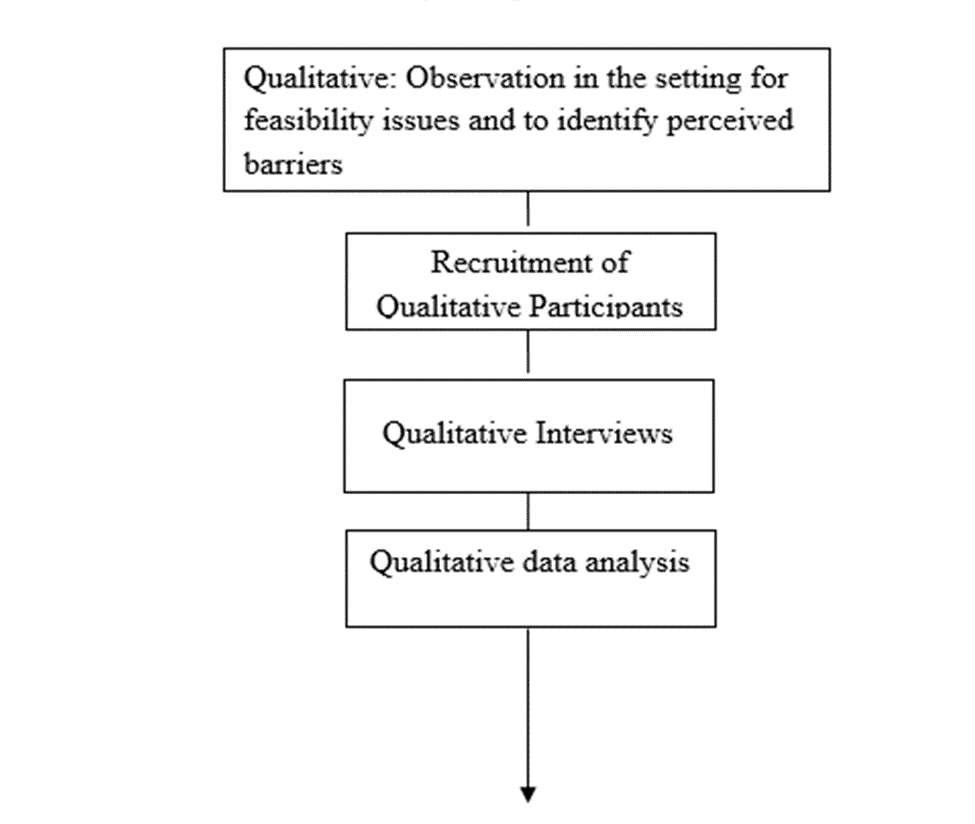 Figure 2: Design and Flow Qualitative Phase.
Figure 2: Design and Flow Qualitative Phase.
Qualitative Observation
Since direct observation is the gold standard to monitor hand hygiene adherence, the researcher observed baseline meal-related hand hygiene behaviors during all three meals over two days. Specifically, the researcher noted whether the residents used a wipe prior to eating, whether they touched their T-zones, and if and how they covered coughs/sneezes. The facility mealtimes included two groups of residents. The first group was independent, while the second group could not independently feed themselves and required assistance to perform hand hygiene.
Adherence was calculated by dividing the number of hand hygiene episodes by the number of opportunities. An episode of hand hygiene referred to the action of cleaning the surfaces of both hands with a disposable wipe. An opportunity referred to pre-meal hand hygiene in the dining hall.
Both the resident and staff samples in the qualitative phase were a purposive sample meeting the following inclusion criteria: can speak English; at least 18 years of age; and able to provide written, informed consent. In addition, the inclusion criteria for the resident sample included a Brief Interview for Mental Status (BIMS) score of 13–15 which indicated intact cognition. The sole exclusion criterion included incomprehensible speech, such as dysphasia. An additional inclusion criterion for the staff member sample was able to provide direct resident care, including assisting with meals. There were no exclusion criteria for the staff sample.
Qualitative Interviews and Analysis
Resident and staff participants’ data were transcribed verbatim and analyzed using the six-step procedure for mixed methods data analysis described by Creswell and Plano Clark (2011). To explore the data, the researcher read the data, wrote memos, and developed a qualitative codebook. The researcher coded the data using procedures recommended by Saldaña (2013), assigned labels to codes, grouped codes into categories, and interrelated the categories into a smaller set of categories. The categories that emerged from the data were as follows: susceptibility to infection, social exposure/social distancing, seriousness of infection, benefits of hand hygiene, barriers to hand hygiene, cues to action, and lack of personal accountability/self-efficacy.
Quantitative Phase
The qualitative findings informed the second phase, which had a quantitative emphasis. The quantitative intervention protocol (Figure 3) was refined based on staff and resident feedback and the researcher’s observation. The schedule for the hand hygiene interventions included the meal-related hand hygiene related behaviors (including respiratory hygiene and T-zone touching) based on the facility’s current practice. The quantitative phase was implemented in three four-day cycles.
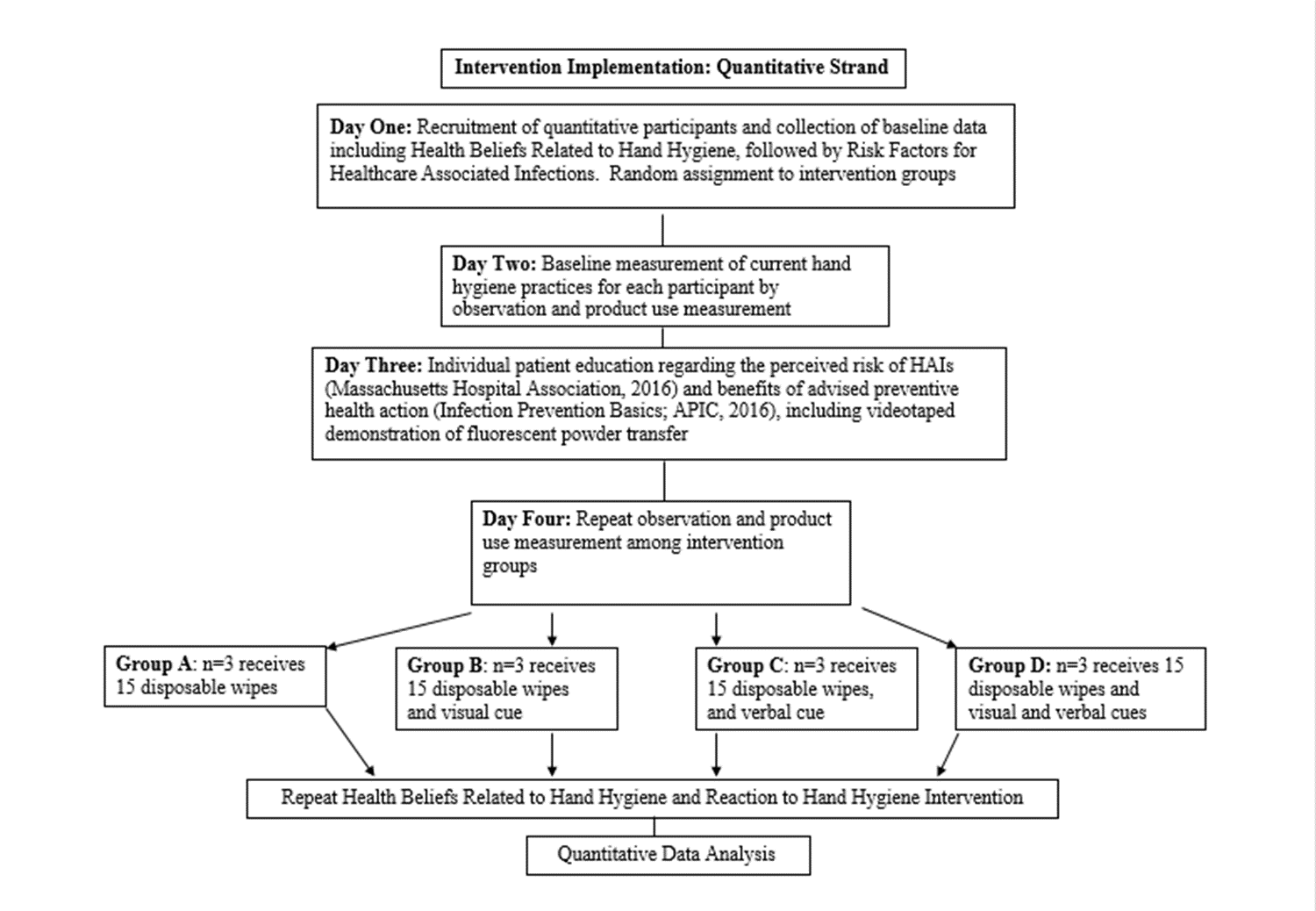 Figure 3: Design and Flow: Quantitative Phase.
Figure 3: Design and Flow: Quantitative Phase.
Quantitative Measurement
On the first day, the researcher completed The Participant Demographics and Environmental Questionnaire (Appendix B) and the Risk for Healthcare-Associated Infection Tool (Appendix C). The researcher also administered The Health Beliefs Related to Hand Hygiene (Appendix D) face-to-face. On the second day, all participants received disposable wipes per the facility’s current practice. The researcher observed episodes of meal-related hand hygiene behaviors throughout the meal. This included verbal cues from healthcare workers. On the third day, participants received education regarding the seriousness of healthcare-associated infections (Massachusetts Hospital Association, 2016). To promote perceived benefit of the advised preventive health action and enhance self-efficacy, participants received the Infection Prevention Basics (APIC, 2016). The individual risk factors for healthcare-associated infections were discussed with the participants. For consistency, education was also presented in a short web-based video. Lastly, participants demonstrated proper hand hygiene with a disposable wipe accompanied by lyrics written by the researcher to the tune of Happy Birthday to time the hand hygiene.
Quantitative Visual Cue
Participants were randomly assigned to receive visual cues. Six participants (n=6) received education, a disposable wipe, and verbal cues per the facility’s current practice. Six participants (n=6) received education, disposable wipe, verbal cues per the facility’s current practice, and a laminated visual cue, which was a triangular table tent placed on the participant’s table (Appendix E). Other tables had a similar table tent with a generic greeting.
Quantitative Data Analysis
The researcher entered the quantitative data into Excel and created a codebook. Dichotomous items were coded 0 for no and 1 for yes. Likert items were scored according to instrument documentation. Quantitative data analysis was conducted using SPSS version 23.0. The researcher entered the data into SPSS, screened the data for errors, and cleaned the data using established protocols (Pallant, 2013). Frequency distributions were calculated for each variable to check the minimum and maximum scores and to assess valid and missing data. Missing data were minimal and assigned the code 999.
Flowsheet for Hand Hygiene Observation
Observation of hand hygiene situations, behaviors, and adherence both prior to and after the intervention were recorded on the Flowsheet for Hand Hygiene Observation. Respiratory hygiene actions included covering a cough or sneeze with anything other than the bare hand. T-zone touching was defined as skin-to-skin contact of the hand with the eyes, nose, or mouth. Wiping the mouth with a napkin was not included as an episode of T-zone touching. Finger licking was included as an episode of T-zone touching. If a participant did not eat a meal in the dining hall, no data were entered for that meal. The data on this tool is at the interval/ratio level. The percentage of adherence to hand and respiratory hygiene was calculated using the conventional method defining the numerator as an observed episode of hand or respiratory hygiene and the denominator as an observed opportunity when hand or respiratory hygiene would be appropriate. For example, if a participant ate all three meals in the dining hall, there were three opportunities for pre-meal hand hygiene. If the participant performed hand hygiene prior to one of those meals, the adherence score would be 0.33. If a participant did not eat a meal in the dining hall, no data were entered for that meal.
Results and Discussion
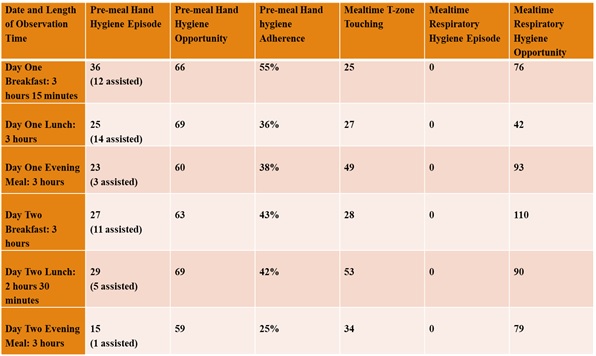
There was a total of 155 episodes and 386 pre-meal hand hygiene opportunities for an overall adherence of 40%. Forty-six of these hand hygiene episodes were assisted by staff. While the researcher’s presence in the dining hall may have initially served as a reminder to perform hand hygiene, pre-meal hand hygiene trended downward from 55% prior to breakfast on the first day of observation to 25% prior to the evening meal on the second day of observation.
Respiratory hygiene involves behaviors associated with coughing/sneezing to prevent the spread of infection. Since it may be difficult for residents to cover coughs/sneezes with their elbow, covering the cough or sneeze with something other than their bare hand was considered acceptable for the study. A bare hand was considered unacceptable as it contaminated the hand and potentiated the spread of infection. Tissues were not provided to the residents in the dining hall; however, disposable napkins were. There were 490 episodes of coughing/sneezing observed. None were addressed by residents using acceptable respiratory hygiene methods (Table 1).
Table 1. Field Observation of Hand Hygiene, T-zone Touching, and Respiratory Hygiene
Qualitative Recruitment
The population size was 150 residents (number of beds in the facility). Participants in the qualitative phase included an equal number of male and female long-term care facility residents and staff members (total n=12).
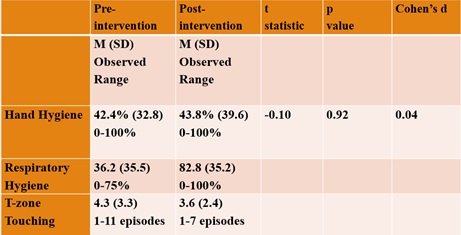
While hand hygiene opportunities were constant for all participants eating in the dining hall, respiratory hygiene opportunities and episodes of T-zone touching varied (Table 2). Although hand hygiene increased minimally, the mean percentage of adherence to respiratory hygiene increased with a decrease in the range of T-zone touching following the intervention. These findings suggest the participants were more aware of the role of respiratory hygiene and T-zone touching in disease transmission after the intervention.
Table 2: Comparison of Adherence to Pre and Post-intervention Meal-related Hand Hygiene Behaviors
Participant Demographics and Environmental Context Questionnaire
The quantitative sample was predominantly female with a mean age of 85 years (Table 3). On average, resident participants resided in the long-term care facility for 2 ½ years. Polypharmacy was noted, with a mean of 14 routine medications (range of 9–23 medications) and a mean of 21 total daily doses of routine medications (range of 7–40 doses) for the sample.
Table 3: Sample Demographic and Clinical Characteristics (n=12)
| Variable | Mean ± SD |
| Age | 84.75 ± 11.55 |
| BIMS score | 14.75 ± 0.45 |
| Number of days in the long-term care facility at time of study entry | 951 ± 1197 |
| Number of routine medications | 14.08 ± 5.27 |
| Number of total daily doses of routine medications | 21.33 ± 10.85 |
| Gender | Frequency (%) |
| Male
Female |
4 (33)
8 (66) |
Risk for Healthcare-Associated Infections tool
While neither the residents nor staff participants recognized the population as inherently at increased risk for infection, the mean score on the Risk for Healthcare-Associated Infections tool for the sample was 7 (range of 4–10); indicating an above average risk for health-associated infections.
The Health Beliefs Related to Hand Hygiene Tool
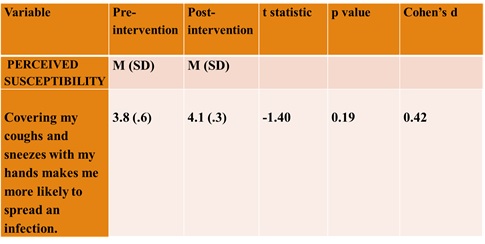
There were medium or large effect sizes noted in all sub-scales of the Health Beliefs Related to Hand Hygiene Tool. One of the six items on the Perceived Susceptibility sub-scale demonstrated a medium effect (Table 4), suggesting participants had an increased awareness of the role of respiratory hygiene in transmission of infection following the intervention.
Table 4. Perceived Susceptibility Sub-scale
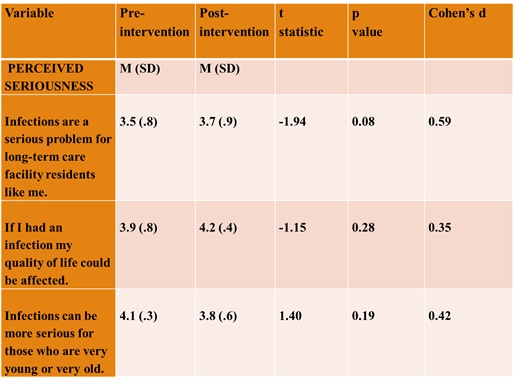
Three of the five items on the Perceived Seriousness sub-scale demonstrated medium to large effects (Table 5), participants had an increased perception of the seriousness of infection and its impact on their lives following the intervention. The item, Infections can be more serious for the very young and the very old, also demonstrated a medium effect. However, the mean decreased suggesting participants had less strong beliefs related to this idea following the intervention. Participants stated they were not sure how to answer this double-barreled item, which may have confounded this result.
Table 5. Perceived Seriousness Sub-scale.
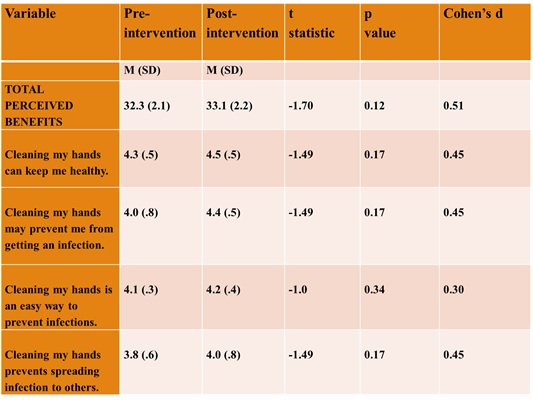
The total score and four of the eight items on the Perceived Benefits sub-scale (Table 6) demonstrated medium to large effects. These findings indicate an increase in positive health beliefs about the benefits of hand hygiene in reducing the risk or seriousness of infection following the intervention.
Table 6. Perceived Benefits Sub-scale
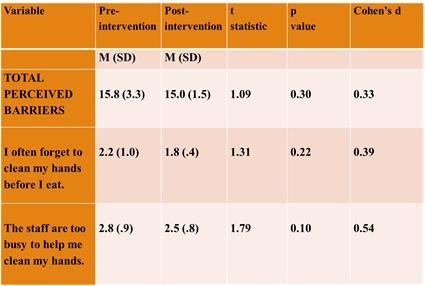
The total score and two of the seven items on the Perceived Barriers sub-scale (Table 7) demonstrated medium to large effects, suggesting the participants’ perceived barriers to hand hygiene were lower following the intervention.
Table 7. Perceived Barriers Sub-scale
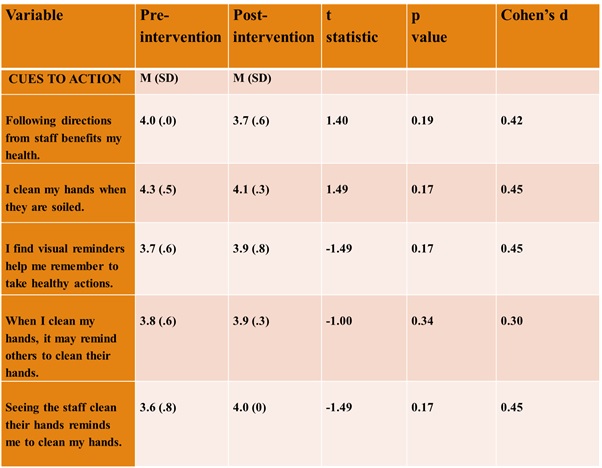
Five of the six items on the Cues to Action sub-scale (Table 8) demonstrated medium effects, however, the direction of the means differed. Beliefs about Cues to Action decreased related to the following items: Following directions from staff benefits my health and I clean my hands when they are soiled. This may be a result of increased self-efficacy. Beliefs about Cues to Action increased for the items, I find visual reminders help me remember to take healthy actions and When I clean my hands, it may remind others to clean their hands. These findings suggest visual cues and peer behavior may positively impact hand hygiene actions.
Table 8. Cues to Action sub-scale
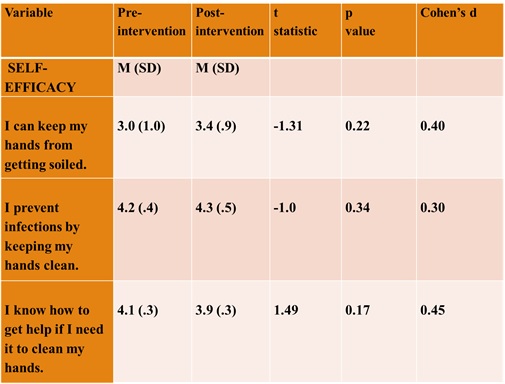
Three of the seven items on the Self-Efficacy sub-scale demonstrated medium effects (Table 9). The changes were positive, indicating an increase in the participants’ confidence in their ability to successfully perform hand hygiene.
Table 9. Self-Efficacy Sub-scale
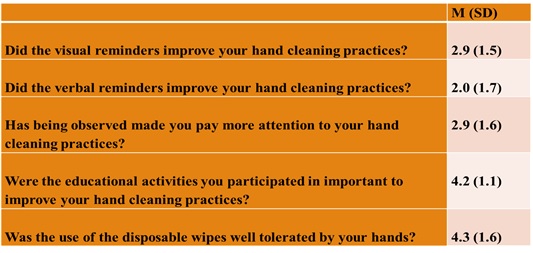
Participant’s Reaction to Hand Hygiene Intervention Questionnaire
Measures of central tendency described the total scale and item-level means on the Participant’s Reaction to Hand Hygiene Intervention questionnaire (Table 10). The three lowest item means were related to agreement that visual and verbal cues and being observed had an impact on hand cleaning practices. The visual cues score on this tool was surprising, as visual cues demonstrated a medium effect on the Health Beliefs sub-scale. However, participants who received visual cues reported a more positive reaction to them. The verbal cue score was not surprising, as no verbal cues from staff were observed during the observation period of the quantitative phase. In addition, with the subjective nature of self-report, participants may have under reported the effect of being observed. The two highest means related to agreement that the use of disposable wipes was well tolerated, and educational activities were important to improve the residents’ hand cleaning practices. These findings suggest the residents tolerated the wipes and valued the educational intervention.
Table 10. Participants’ Reaction to the Hand Hygiene Intervention
Conclusion and Significance
While neither the residents nor staff participants in the qualitative phase recognized the population as inherently at increased risk for infection, the quantitative findings suggest that following the intervention, participants had an increased perception of the seriousness of infection and its impact on their lives. The quantitative findings also indicated participants had positive health beliefs about the benefits of hand hygiene in reducing the risk or seriousness of infection and lower perceived barriers to hand hygiene following the intervention. While participants had to be able to perform hand hygiene independently to meet inclusion criteria for the quantitative phase of the study, two items in the Perceived Barrier subscale (Table 7) focused on the behaviors of others (the staff) rather than the participant.
The study supported findings by Whitby et al. (2008) that elective hand hygiene was predicted by visual cues and peer behaviors. Although the researcher’s presence may have served as a visual cue for all residents, participants reported they were not aware of the researcher’s presence. A negative cue to action may include routine disclosure of healthcare-associated infections or hand hygiene adherence rates within the facility. In addition, recognition of champions of excellent hand or respiratory hygiene each month may serve as cues and improve practice.
The quantitative findings indicate an increase in the participants’ confidence in their ability to successfully perform hand hygiene. A resident-focused hand hygiene intervention may engage and empower residents to become partners in ensuring safety. The hand hygiene intervention is a cost-effective means to actively promote self-efficacy rather than passive reliance on healthcare staff to assure clean hands during meals. As a result, hand hygiene should be included on the Rights and Responsibilities of Residents of Long-Term Care Facilities as part of the expectation for high quality care, a clean and safe environment, and involvement in care.
Obtaining the Sample
No major revisions were identified based on the recruitment strategies, willingness of residents to consent or be randomized, and the number of eligible participants given inclusion/exclusion criteria in the feasibility study. Only one resident was excluded from the qualitative phase due to incomprehensible speech. While there was a 100% overall recruitment rate for the qualitative strand for staff and residents, there was a 70% response rate for recruitment to the quantitative strand of the study. Thirty percent of the residents who were approached to participate declined to participate due to the researcher’s anticipated time commitment, which was originally estimated to be 60 minutes per encounter. However, the time commitment was ultimately determined to be approximately 15 minutes per encounter. Eleven of the twelve participants completed the study, resulting in an 8% attrition rate.
In addition, a selection bias may have affected the results of the Perceived Seriousness and Perceived Susceptibility subscales of the Health Beliefs Related to Hand Hygiene Tool. For example, while the qualitative findings suggested both resident and staff participants expressed a greater recognition of personal risk if their medical history included experience with infections, none of the participants in the quantitative strands had a history of healthcare-associated infections. Furthermore, the mean age of participants in the quantitative strand was 85 and the mean time in facility was 2 years. Participants may have had less awareness of their susceptibility to a serious risk as they had already exceeded the average life expectancy when they entered the facility (average age: 83).
Implementing the Intervention
Since some families ate in the dining hall with the residents, it is recommended in the future pilot study that the family should be included in the educational activity. For future studies, consideration of the preferred method of hand hygiene for the population may ensure success for the hand hygiene intervention. The researcher did not ask participants about their preferred method of hand cleansing prior to the intervention. However, the researcher asked participants at the completion of the study. Three participants preferred alcohol-based handrubs, with one having a container clipped to her walker. Eight participants preferred soap and water, and one preferred a wipe. Of the eight who preferred soap and water, six found wipes an acceptable alternative. Two found wipes unacceptable, stating the wipes left their hands wet and sticky. One participant stated the wipes did not offer any antibacterial benefit, “Wipes don’t have disinfectant. They are just wet.”
In addition, to incorporate a resident-focused hand hygiene program in the mealtime routine, a standard method of delivery is needed. When staff forgot to provide wipes, residents did not ask for them. Placing wipes on top of the plate cover could warm the wipe and ensure all residents would receive a warm wipe with the meal tray. Alternatively, the delivery of the wipe could be cued to donning the clothing protector, as 100% of residents complied with this. However, the wipe should not be placed on top of the clothing protector, as participants were uncomfortable with the resulting dampness. In the future pilot study, it is recommended a greeter or free-standing unit with wipes and/or or alcohol-based handrub be placed in the dining hall entry to accommodate multiple preferences of hand hygiene.
Developing the Best Study Materials
The following should be added to the top of each tool for accurate identification and record keeping: participant identification number and date. Similarly, a box to check if the tool was administered pre-or post-intervention should be added to the Health Beliefs Related to Hand Hygiene Tool and the Flowsheet for Hand Hygiene Observation. When administering the tools, participants who are roommates should be separated when completing questionnaires, as spouses tended to answer for one another when they were in the same room during the feasibility study. Specific recommendations for revision and/or psychometric development for each tool based on use in this feasibility study will be detailed below.
Health Beliefs Related to Hand Hygiene Tool
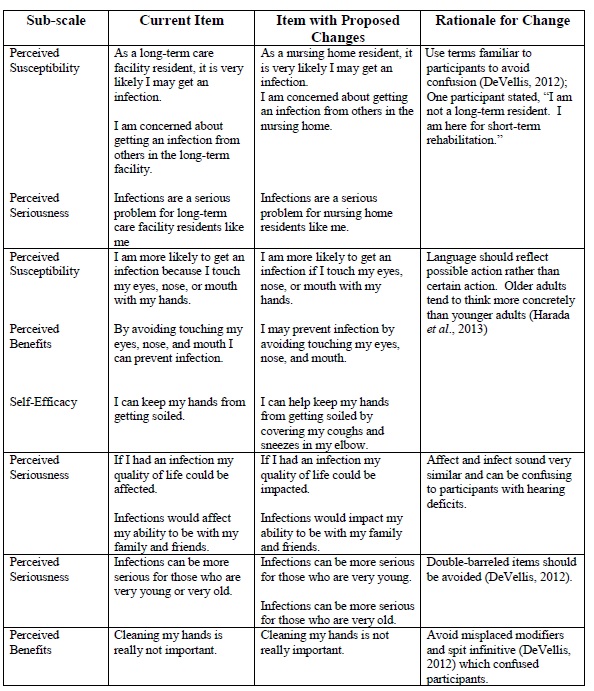
Revisions to the Health Beliefs Related to Hand Hygiene Tool are reported in Table 11 below. Revisions include using terms familiar to participants to avoid confusion and language to reflect possible, rather than, certain action. In addition, revisions should include avoiding terms which sound similar, double-barreled items, and misplaced modifiers. Since older adults tend to think more concretely than younger adults, participants voiced the desire to score each item dichotomously as true or false, rather than on the 5-point Likert scale. Consideration should be given to changing the response option to a dichotomy. Although the statistical analysis was weak due to the small quantitative sample size, preliminary analysis suggested removing the second item in the Cues to Action sub-scale (I clean my hands when they are soiled) may increase scale reliability by increasing the Cronbach’s alpha to 0.743 (pre-test) or 0.693 (post-test).
Table 11. Recommended Changes to the Health Beliefs Sub-scales
 Participant’s Reaction to Hand Hygiene Intervention
Participant’s Reaction to Hand Hygiene Intervention
The instructions for the Participant’s Reaction to Hand Hygiene should be revised from “Instructions: Please indicate how strongly you agree or disagree with each of the following statements by checking the box following the option which best indicates your response” to “Instructions: Please indicate your response to each of the following questions by checking the box following the option which best indicates your response.” Since increased length is associated with increased complexity and decreased clarity, the following revision is suggested for the third item in the Self-Efficacy subscale: “Were you more aware of preventing infection by cleaning your hands during the program?”
Provide the Most Robust Statistical Analysis
Limitations of the feasibility study include not being designed or powered for the researcher to perform statistical hypothesis testing (Lancaster, 2015). However, the study permitted estimation of Cohen’s d effect sizes, which will inform researchers in determining sample size for further studies. The quantitative sample size of 12 was not large enough to estimate Cronbach’s alpha accurately. The use of convenience sampling at a single site for the quantitative phase creates the possibility the sample is not representative of the targeted population.
Overall, the general area of focus for this feasibility study included identifying the most appropriate outcome measures to develop a pilot study. The outcome focus was whether hand hygiene was performed. The study did not attempt to quantify how well the residents cleaned their hands or colonization of hands with bacteria. However, this was a feasibility study, and methodological decisions such as convenience sampling, sample size, and the use of a single site were based on practical constraints such as access to participants, time, and resources.
In conclusion, findings from both the quantitative and qualitative strands provide key information for future piloting of a resident-focused hand hygiene intervention on a larger scale.
The feasibility study informed the optimal ways to obtain the sample, implement the intervention, develop the best study materials, measure variables, and have the most robust statistical analysis. The recruitment strategies, willingness of residents to consent or be randomized, and the number of eligible residents given inclusion/exclusion criteria suggest the hand hygiene intervention is appropriate for pilot testing. The study provided insight into optimal approaches for pilot testing the resident-focused hand hygiene intervention. The study yielded useful data to direct tool revision and future studies. Recommendations for future research include using the methods and steps in this feasibility study in a pilot study. Lastly, the study permitted estimation of Cohen’s d effect sizes which will inform researchers in determining sample size for further studies.
Appendix
→ Click here to download the supporting Appendix
References
Association for Professionals in Infection Control and Epidemiology. (2014). Infection prevention basics. Retrieved from http://consumers.site.apic.org/infection-prevention-basics/
Benner, P. (1984). From novice to expert, excellence and power in clinical nursing practice. Menlo Park, CA: Addison‐Wesley Publishing Company
Burnett, E., Lee, K., & Kydd, P. (2008). Hand hygiene: What about our patients? British Journal of Infection Control, 9, 19-24.
Centers for Disease Control. (2016). National and state healthcare-associated infections progress report. Retrieved from: http://www.cdc.gov/hai/progress-report/index.html.
Champion, V. L. (1984). Instrument development for health belief model constructs. Advances in Nursing Science, 73-87.
Creswell, J. W., & Plano Clark, V. L. (2011). Designing and conducting mixed methods research (2nd ed.). Los Angeles, CA: Sage.
DeVellis, R. F. (2012). Scale development: Theory and applications. Thousand Oaks, CA: Sage.
Harada, C. N., Natelson Love, M. C., & Triebel, K. (2013). Normal cognitive aging. Clinics in Geriatric Medicine, 29, 737–752. http://doi.org/10.1016/j.cger.2013.07.002
Kretzer, E., & Larson, E. (1998). Behavioral interventions to improve infection control practices. American Journal of Infection Control, 26, 245-53. doi:10.4103/0972-5229.78215
Kris, A.E., (2015). Gerontological nurse certification review. (2nd ed.). New York, NY: Springer Publishing Company.
Lancaster, G. (2015). Pilot and feasibility studies come of age! BioMed Central. Retrieved from https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/2055-5784-1-1
Lawrence, M. (1983). Patient hand hygiene: A clinical enquiry. Nursing Times, 79, 24–25.
Massachusetts Hospital Association, (2016). Healthcare-associated Infections. Patient CareLink. Retrieved from http://patientcarelink.org/improving-patient-care/healthcare-acquired-infections-hais/
Office of Disease Prevention and Health Promotion. (2013). National action plan to prevent health care-associated infections: Road map to elimination. Retrieved from http://www.health.gov/hcq/prevent_hai.asp#hai_plan
Pallant, J. F. (2013). SPSS survival manual: A step by step guide to data analysis using SPSS for Windows. Crows Nest, N.S.W: Allen & Unwin.
Polit, D. E., Beck, C. T., & Owen, S. (2007). Focus on research methods: Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Research in Nursing & Health, 30, 459-467
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education Monographs. 2,328–335.
Rosenstock, I. M. (1990). The health belief model: Explaining health behavior through expectancies. In K. Glanz, F. M. Lewis, & B. K. Rimer (Eds.), Health behavior and health education: Theory, research, and practice. 39-62. San Francisco, CA: Josey-Bass.
Saldaña, J. (2013). The coding manual for qualitative researchers (2nd ed.). Los Angeles, CA: Sage.
Smith, P., Bennett, G., Bradley, S., Drinka, P., Lautenbach, E., Marx, J., … Stevenson, K. (2008). Guideline: Infection prevention and control in the long-term care facility. American Journal of Infection Control, 36, 504-535.
Whitby, M., McLaws, M. L., Slater, K., Tong, E., & Johnson, B. (2008). Three successful interventions in health workers that improve compliance with hand hygiene: Is sustained replication possible? American Journal of Infection Control,36:349–55.
World Health Organization. (2009). WHO Guidelines for hand hygiene in health care. Retrieved from http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf












