Abstract
Since December 2019, the novel coronavirus, SARS-CoV-2, has spread across the world, wreaking havoc on a global scale that has devastated economies and taken a serious human toll. While vaccines have been approved, it will take time to deploy them to a global population and reach herd immunity. Moreover, newer, more transmissible variants are being discovered frequently and fueling a surge in cases that requires vigilance in the months to come to ensure we are reducing the spread. Throughout this period employers have faced a number of difficult decisions, including whether to close their doors or remain open and take on the added risk of exposure to their employees and customers. The pandemic has been particularly challenging for essential services that must find ways to continue to operate while keeping their employees and patrons safe. To keep our economy open and our communities safe in this challenging environment, we need to be able to make informed decisions, backed by scientific evidence.
Environmental monitoring for SARS-CoV-2, the virus that causes COVID-19, allows us to determine the presence of the virus in the environments in which we live, work, and play. The gold-standard qPCR-based testing method uses the same principles applied in clinical tests with results in under two hours. This non-invasive testing method provides two key types of information: (1) that the virus is/was present in the space, and (2) that an infected person (potentially presymptomatic or asymptomatic) has passed through since it was last disinfected.
This knowledge can lead to a variety of crucial actions, like closing off impacted sections, deep cleaning and disinfection, contact tracing those at risk of infection, and clinical testing. These actions can mean the difference between successfully staying open or risking future recurring or prolonged closures due to widespread community spread.
Main Article
Are we using all the tools at our disposal to stop the spread of COVID-19?
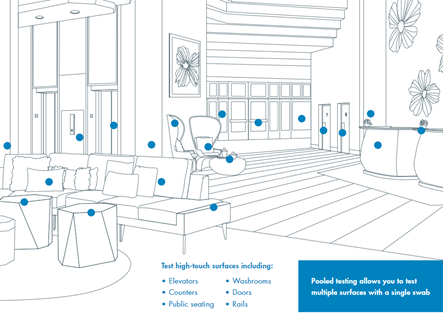
The ability to identify the lingering presence of SARS-CoV-2 on high-touch surfaces, like elevator buttons and door handles, or in the air and water provides crucial early knowledge that is essential to keeping the workforce safe. The presence of the virus in a facility indicates that it was brought in by someone and poses a risk that should be mitigated.
While we are all now familiar with clinical testing and contact tracing of individuals to limit the spread of COVID-19, it can take days to weeks for symptoms to appear and an outbreak to be recognized. These days and/or weeks between exposure and clinical diagnosis present ample time for the virus to run rampant in a community, quickly overwhelming public health capacity and resulting in strict lockdowns to quickly slow the spread. Environmental surveillance testing is non-invasive and allows for immediate detection of SARS-CoV-2 in environments, which can prompt crucial actions to mitigate risk, reduce spread, and help the economy stay open amidst inevitable flareups.
What is environmental surveillance testing?
Environmental surveillance testing uses the same quantitative Polymerase Chain Reaction (qPCR) technology as clinical diagnostics to test surfaces for the presence of SARS-CoV-2.
This testing method is not new; it has been used for decades to monitor for pathogens and biothreats in industries like healthcare and food production and has been used in the manufacturing industry to keep employees safe, monitoring for threats such as Legionella. This testing method is now available to quantify the risk of SARS-CoV-2 on nearly any surface that we encounter, with the results available in under two hours.
tested at the end of each shift or workday, before cleaning and disinfection
High-touch surfaces, like elevator buttons, door handles, railings, and bathroom faucets, could be tested at the end of each shift or workday, before cleaning and disinfection. If a result comes back positive, it indicates that someone with the virus was present in the facility during that specific window of time.
Decision-makers are then armed with the information they need to take next steps, like closing off sections, deep cleaning and disinfection, contact tracing those who may have been exposed, and clinical testing of individuals. This quick, corrective action can prevent a potential outbreak before it has time to spread.
How does it work?

Samples from high-touch surfaces are collected using a swab, and then immediately placed into a tube containing a proprietary preservation buffer, inactivating any viable virus. This preserves the viral RNA until later testing and enables storage and transportation at room temperature.
The viral RNA is placed into a qPCR device for analysis where it is reverse-transcribed into complementary DNA. If the virus is present, primers that specifically match SARS-CoV-2 targets combine with the transcribed DNA, allowing it to be amplified through a series of PCR cycles.
These amplified products also produce a fluorescent signal, which is monitored during each PCR cycle. Results are reported automatically at the end of the process. Sensitive, objective, rapid, and specific results are why qPCR testing is the gold standard to assess and manage risk.
Keep employees safe with regular non-invasive testing
Testing each employee every day for COVID-19 is challenging, costly, and invasive. Consistent environmental surveillance testing of high-touch surfaces can provide an overall picture of the health of a facility and can be easily integrated into existing protocols.
A proactive approach to monitoring for early warning signs indicates to stakeholders that their safety is taken seriously and that the facility’s managers are actively working to mitigate risk.
Identify early warning signs
With a consistent testing protocol, early warning signs of an outbreak can be identified with a specific timeframe of virus introduction.
This critical information empowers decision-makers to take additional investigative actions to make informed decisions, including more accurate contact tracing to identify people for clinical testing. Early warning signs can help mitigate the risk of transmission and the need to wait for symptoms to appear.
Avoid costly shutdowns
There is power in being able to get ahead of a situation before it is out of control. Identifying asymptomatic and presymptomatic cases is critically important, as research has shown that 44% of human-to-human transmission occurs when the initial case is presymptomatic (He, 2020). In a new reality that seems out of our control, environmental surveillance testing is a tool to ensure that facility managers are in command of their business.
When a temporary worker at one of Illinois’ largest meatpacking plants tested positive for COVID-19, the plant was able to avoid a shutdown, in part because they had been consistently conducting environmental surveillance testing through a local university and had not received any positive results. Additionally, they were able to show regulatory bodies that they had been following infection control practices (Dempsey, 2020).
Environmental surveillance testing provides timely information and enables the quick responses required to keep businesses open.
Restore public confidence
Environmental surveillance testing not only allows for the detection of SARS-CoV-2, but also helps to restore confidence amongst the public and employees by demonstrating that every tool available has been implemented in an effort to keep employees and communities safe.
Identify the virus, stop the spread
We need to think differently about pandemic management. Even while the vaccine rolls out, there remains a need for vigilance to ensure that we effectively reduce the spread. As opposed to conducting daily, invasive clinical tests on every employee, surface testing is a cost-effective, non-invasive, simple, and accurate way to perform ongoing surveillance of the health of a facility and the people within it.
This technology is part of the TIPS Science to Market® Program
Contact the TIPS team for more information
References
Dempsey, P. (2020, July 03). COVID-19 REPORT: Temporary worker at meat processing plant tests positive for Covid-19. From: https://www.rantoulpress.com/coronavirus/covid-19-report-temporary-worker-at-meat-processing-plant-tests-positive-for-covid-19/article_39ed23b4-bd7a-11ea-ae5e-fbc85e631673.html
He, X., Lau, E., Wu, P., Deng, X., Wang, J., Hao, X., . . . Leung, G. (2020, April 15). Temporal dynamics in viral shedding and transmissibility of COVID-19. From: https://www.nature.com/articles/s41591-020-0869-5












