Abstract
The good news is that there are now two effective COVID-19 vaccines now available in the USA, one from Pfizer and the other from Moderna. The challenge now is to overcome the politicization of the COVID-19 response and any reluctance to be immunized. Several strategies are presented here.
Main Article
We’ve had great news this past week, with two COVID-19 vaccines getting Emergency Use Authorizations (EUA) from the FDA. The first shipments of vaccines from Pfizer have been sent across the USA, landing primarily in urban areas and larger hospitals that have the ultra-cold freezers needed for storage. Moderna has also started shipping vaccines, which are easier to store, so will be sent to smaller hospitals and communities as well.
The rollout has had many glitches. For example, there has been considerable acrimony over who gets the first shots since there is a limited supply of the vaccine. Many argue health care workers should be first, others that elderly nursing home residents should have priority since they have the highest death rate (Zeynep, 2020).
One of the biggest problems is that the COVID-19 vaccine has been so politicized. Getting people to trust and accept it is a surprisingly tall hurdle.
Communications scientists are tackling that task and trying test messages. I’ve been text banking for the elections all fall and have seen how campaigns try slightly different messages to potential voters. Then, based on feedback and response rate to the different messages, they adapt the message to optimize its effectiveness. It’s very much the same with vaccines.
Recent polls show significant reluctance of the public to be vaccinated, especially among women (Kahn, C. and Beasley, D., 2020)
What are some of the issues we need to address?
The first is the politicization of public health measures to control the virus. Those who refused to wear masks and decried scientists and doctors as just being greedy may be more reluctant to receive vaccines. This even extends to conspiracy theorists who claim the shots are being used to microchip people.
With the country so bitterly divided, naming a research and development campaign “Operation Warp Speed” was not the best messaging. It suggested to many, myself included, that President Trump would cut many corners to have a successful vaccine candidate announced before the November election. In its messaging, Pfizer emphasized that it was not a part of Warp Speed and that its research was independent of government funding. Moderna’s candidate came with baggage because its CEO, Moncef Slaoui, refused to divest himself of stocks and had a gross conflict of interest (Arnsdorf, 2020).
For me, and many in my circle, the science prevailed. The companies have been unusually transparent in posting their protocols on the web for anyone to examine. The FDA Advisory Committee meetings were broadcast and hundreds of pages of reports were made public. The safety profile has thus far been excellent and the efficacy astonishing. Initially, the FDA and NIH hoped for a 50% efficacy, comparable to that for influenza vaccines. Instead, both of these vaccines appear to provide about 95% protection and I have become an enthusiastic proponent. When fielding questions from my family and community, I ask people what their concerns about it are. Then we talk about the risks and benefits of vaccination vs. a COVID infection. The talk is usually quite brief when people put the small risks of vaccination in perspective to the pandemic.
Some of the remaining issues that need to be addressed include:
Is the vaccine safe for pregnant women and children? So far, there have been no problems seen in women who are pregnant or breastfeeding. Animal studies are not raising any concerns either. Human studies will be ongoing, and there are vaccine registries to capture any bad outcomes. Studies with children age 12 and older are beginning now. Presumably, after that, they will study the vaccine in younger kids.
How do we overcome the spectrum of those reluctant to have vaccinations—ranging from vaccine-hesitant (who have legitimate questions or concerns and are awaiting more information) to antivaxxers, who adamantly reject all vaccines? We still have not recovered from Andrew Wakefield falsely claiming that the measles/mumps/rubella vaccine causes autism. Prominent actors amplified these lies. The result? Vaccine refusal and outbreaks of measles throughout the USA and Europe. Physicians and public health officials who promote vaccination also received death threats.
Perhaps the biggest reluctance will surround issues of race. There is, understandably, a long-standing legacy of mistrust from Black communities, given the history of civil rights abuses and unethical studies. The most well-known abuses are the Tuskegee syphilis study and the story of Henrietta Lacks (CDC, 2020). The level of mistrust has only been heightened by the murders of George Floyd, Breonna Taylor, Ahmaud Arbery and so many others, as well as by the crackdowns on the peaceful and growing demonstrations protesting that Black Lives Matter.
With COVID-19, Blacks, Latinos, and Native Americans have had a far greater proportion of illness and death. Some of this may be due to genetic variations (Peter Baillie’s group is finding mutations that help predict the severity of disease). More is likely due to “social determinants of health”—disparities because of being more likely to live and work in crowded conditions and being unable to work remotely, for example (Riley, 2020). The outbreaks of COVID-19 in meatpacking plants and in prisons are two stark examples of the disparities.
Strategies to overcome mistrust and increase uptake
The most important strategy is to build trust. This includes having a public, expert-driven allocation of vaccines for fairness and equitable access.
Another strategy for the general public is showing prominent people receiving vaccinations on television. Of course, some question why politicians who are not in a high-risk group and who have been outspoken opponents of masking and public health campaigns, should “jump the queue” and be vaccinated before health care workers and nursing home residents but many people who are vaccine-hesitant have said they would take the vaccine when Dr. Fauci said that he thought it was ok. He just received the Moderna vaccine; President-elect Biden was given Pfizer’s.
Twitter has had some powerful threads from prominent Black physicians getting vaccinated, e.g., this from Alden Landry:
“Let’s set the record straight. The health care workers taking pics and posting/tweeting about receiving their vaccine aren’t bragging and being boastful about being first. We’re saying we trust science. We’re grateful for the glimmer of hope in this pandemic,” (Landry, A. 2020)
This, from UCLA’s Medell Briggs, was another excellent message.
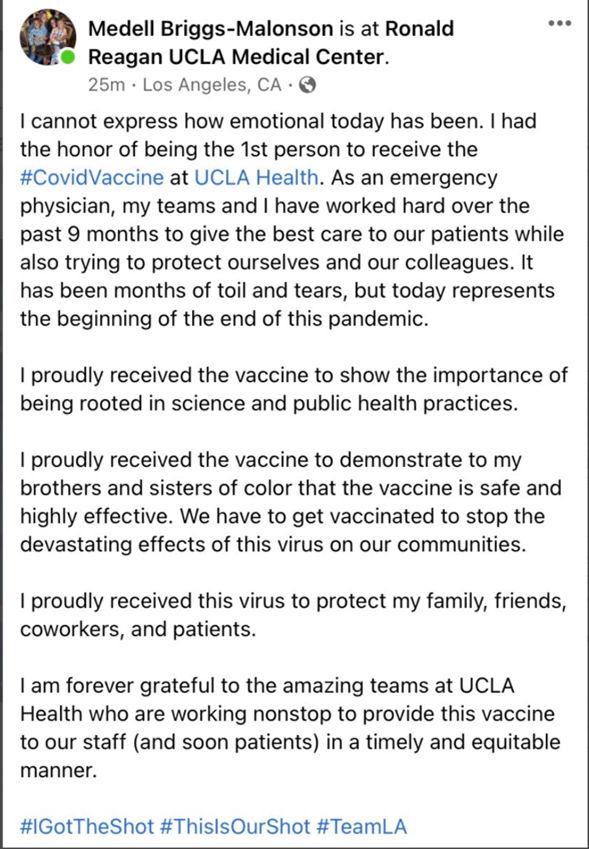
(Blackstock, U. 2020)
And Dr. Fauci highlighted that Dr. Kizzmekia Corbett, a young Black female scientist, led the development of the Moderna vaccine at NIH (Mahadevan, (2020).
Similarly, Dr. Michelle Lopez was the first to be vaccinated in the Rio Grande Valley. She said, “I hope that our community will actually listen to science, and not memes on Facebook.” The accompanying photos showed her as a physician and a mother of young children (Colon, 2020).

There are many other examples of leaders modeling good communication in reassuring others that it is safe to be vaccinated. The CDC offers some specific messaging, if needed.
It is essential that the CDC and government set accurate expectations for the vaccine, and especially that they warn people that there are expected, normal but unpleasant side effects of the vaccine, including fever and achiness, which are signs of your body mounting a good immune response. They also are educating the public that they are monitoring for new or unexpected side effects. For example, the serious allergic reactions were picked up by the Vaccine Adverse Events Reporting System, which illustrates that it is working. A further major educational effort also needs to be devoted to getting people to understand that we will still need to wear masks, socially distance, wash and /or sanitize our hands, etc., until the time arrives when most of us have been vaccinated.
We have several hurdles to overcome for broad vaccine acceptance. As COVID-19 cases explode now after the holidays and more families are hurt by the trauma of the infection and deaths or long-term disability, I would expect there to be a growing enthusiasm for the vaccine. Some of the hesitation over the MMR, for example, is undoubtedly because hardly anyone has witnessed the infections that preceded the vaccine era. Losing loved ones will starkly illustrate the risk-benefit ratio and increase acceptance.
We need to publicly reward vaccination with stickers and perks, perhaps access to live entertainment in the future.
Let’s make becoming immunized the norm and the cool thing to do!
References
Arnsdorf, I. (2020) Trump’s Vaccine Czar Refuses to Give Up Stock in Drug Company Involved in His Government Role. propublica.org; Accessed Dec 22, 2020. https://www.propublica.org/article/trumps-vaccine-czar-refuses-to-give-up-stock-in-drug-company-involved-in-his-government-role
Blackstock, U. (2020) Twitter.com, Accessed Dec 22, 2020. https://twitter.com/uche_blackstock/status/1339329827216625666?s=20
CDC. (2020) How to Build Healthcare Personnel’s Confidence in COVID-19 Vaccines. cdc.gov, Accessed Dec 22, 2020. https://www.cdc.gov/vaccines/COVID-19/downloads/Build-Healthcare-Personnel-Confidence.pdf
CDC. (2020) U.S. Public Health Service Syphilis Study at Tuskegee. cdc.gov, Accessed Dec 22, 2020. https://www.cdc.gov/tuskegee/timeline.htm
Colon, C. (2020) Twitter.com, Accessed Dec 22, 2020.
https://twitter.com/ColonCJC/status/1339237738965561345?s=20
Kahn, C. and Beasley, D. (2020) More women than men in U.S. nervous about fast rollout of COVID vaccine, and that’s a problem: Reuters/Ipsos poll; reuters.com, Accessed Dec 22, 2020. https://www.reuters.com/article/health-coronavirus-vaccine-poll/more-women-than-men-in-u-s-nervous-about-fast-rollout-of-COVID-vaccine-and-thats-a-problem-reuters-ipsos-poll-idUSKBN28L0F3
Landry, A. (2020) twitter.com. Accessed Dec 22, 2020.
https://twitter.com/AMLandryMD/status/1339358204531265542?s=20
Mahadevan, T., (2020) complex.com, Fauci Spotlights Dr. Kizzmekia Corbett, the 34-Year-Old Black Woman at the Forefront of COVID Vaccine Development. Accessed Dec 22, 2020. https://www.complex.com/life/2020/12/fauci-spotlights-dr-kizzmekia-corbett-black-woman-COVID-vaccine-development?
Riley, L. (2020) rutgers.edu, More Than Words: Communicating About a COVID-19 Vaccine. Accessed Dec 22, 2020. https://globalhealth.rutgers.edu/news/more-than-words-communicating-about-a-COVID-19-vaccine/
Tufekci, Z. (aka Zeynep). (2020) substack.com, Will the U.S. Snatch Defeat From the Jaws of Vaccine Victory? Accessed Dec 22, 2020. https://zeynep.substack.com/p/will-the-us-snatch-defeat-from-the?utm_medium=email&utm_campaign=cta