Abstract
The COVID-19 pandemic is one of the deadliest in modern history, quickly spreading to every corner of the globe and causing major health and economic damage in its wake. Despite best efforts, global consensus on the most effective methods to mitigate, control and contain the disease while balancing societal freedoms has been lacking. Add to that misinformation and a lack of scientific consensus among leading organizations on the best approaches to take and it quickly becomes apparent why there is a very real disconnect between those nations that have effectively contained the virus and those that have not.
With no clear blueprint for success, there is an opportunity for science-guided, informed, and effective decision-making to lead the charge in the fight against COVID-19. Objective data that can help locate and quantify the risk posed by COVID-19 is imperative and sorely needed, but currently access to this data is limited to government health agencies that are understaffed and under-resourced. Using every available tool to locate and contain the virus is the best opportunity to avoid mass-scale lockdowns. The gold-standard qRT-PCR method for viral detection, while not perfect, is the best tool we have to detect the virus with sensitivity and specificity. However, relying on clinical diagnostic testing alone to identify COVID-19 strains the healthcare system and often is a reactionary measure that detects the disease after potential outbreaks are well underway. Broadening the scope and use of qPCR testing to include proactive surveillance of the environment, including surfaces and wastewater, may be the missing link in the disease containment strategy.
Main Article
The novel Coronavirus (SARS-CoV-2), first detected in Wuhan China in December of 2019, has since travelled to over 216 countries, wreaking havoc on a global scale that has taken an extreme human toll. Viral spread has been rapid, mostly because no human had previously been exposed to the unique strain, leaving immune systems under-prepared for the upper respiratory onslaught that has proven deadly, specifically for vulnerable segments of the population including the elderly, immunocompromised and some underserviced and minority populations (Moore et. al, 2020, Alcendor, 2020).
Successful strategies during the first wave
Success stories in the face of a pandemic are hard to quantify, particularly while it is occurring, but in general those countries that have been able to strike the balance of protecting their citizens from disease, while at the same time balancing economic activity and a social safety net are viewed as the most successful. The countries that have done well thus far, as measured by low number of cases, deaths, and economic help for those that need it, include: South Korea, Taiwan, Singapore, New Zealand, Australia, Canada, Germany, and Iceland (TIME, 2020).
The overall strategy for successful countries has included border closures and mandatory quarantines for international travelers, aggressive symptom monitoring, physical distancing and community face masks combined with targeted testing of suspected COVID-19-positive cases and isolation for their close contacts. Rapid and widespread clinical testing is an important part of limiting disease spread.
Reopening Challenges
Opening and Staying Open
Lockdowns that restrict local activity to only essential services and travel have been implemented in some jurisdictions to try to slow the spread of the virus and ensure that hospitals do not become overwhelmed by excess patient load. In effect, locking down entire communities signals a defeat of control measures and is a last resort effort to limit further viral spread.
Due to the severe economic and social impacts of lockdowns, which are sometimes viewed as greater than the impact of the virus itself, lockdown measures are often lifted as the result of public pressure. Some areas have opted to remain open in the face of rampant viral spread, resulting in record high cases and extreme mortality rates (NEJM, 2020). When confronted with this reality, we must re-examine the strategies and identify the missing links in disease prevention.
There have been several challenges with COVID-19 management to date, including: 1) the lack of clarity on all potential transmission modes; 2) the underestimation of silent spread of the disease through asymptomatic and pre-symptomatic transmission; and 3) the lack of availability and resources for population-wide testing to identify 1 and 2 above.
The best strategies to control COVID-19 have utilized a mix of technology for rapid diagnosis and isolation of infected individuals to contain outbreaks, followed by rapid contact tracing to isolate exposed and potentially infective contacts to best protect the most vulnerable members of the population (Roncha, 2020, Sheikh et al., 2020).
Transmission Modes Not Fully Understood
SARS-CoV-2 transmission can occur through several routes, like other respiratory viruses as reviewed in Otter et al., 2016 (See Fig. 1). The focus to date has been on human-human transmission through droplet formation by an infected individual and the direct transmission of that material to uninfected individuals. Early pandemic responses emphasized the predominant role of droplets (>5µm) in the spread of the virus rather than aerosols (<5µm), primarily since early data suggested close contact was the predominant route of transmission for the disease. While governing organizations have stated that the primary route of transmission is through direct inhalation of droplets or indirect contact with droplets followed by transfer through the mucous membranes, there is growing evidence and suspicion that smaller droplets (aerosols) may remain airborne for longer and these may be vectors for direct transmission through inhalation (Morawska and Cao, 2020, Godri et al., 2020). Indeed, the CDC and WHO have both stated that aerosol transmission is possible and should be looked at further as a contributing factor in SARS-CoV-2 transmission (CDC, 2020). While airborne transmission may be most likely occurring through droplet formation and transmission between humans in close contact, further risk is present for aerosol transmission particularly in enclosed spaces, with prolonged exposure to respiratory particles and in areas with poor ventilation or air handling (CDC, 2020). This is a primary concern for the hospitality industry, recreational facilities and office buildings that are predominantly indoor facilities where large groups congregate in close quarters. Examples include office buildings with many high frequency touchpoints, apartment buildings, recreational venues, hospitality venues, travel and transportation vessels and buildings. These locations are prime environments for super-spreader events and represent the biggest challenge to re-opening plans. With the increased risk for potential outbreaks comes the need for additional mitigation strategies to reduce the risk. In these cases, extra precautions should be taken to ensure transmission through surfaces and air are minimized.
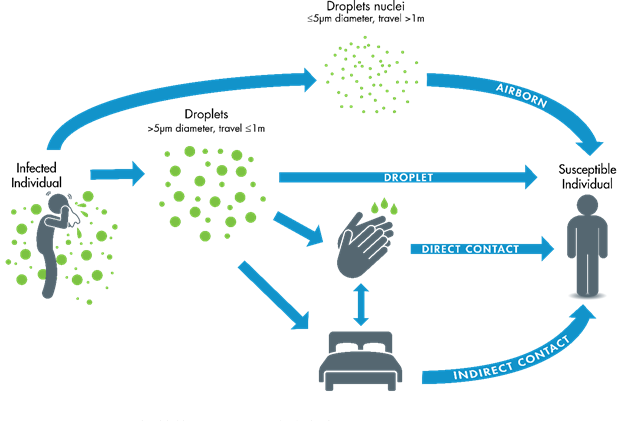
Figure 1: Transmission routes for respiratory viruses, including SARS-CoV-2 (Otter et al., 2016)
The Persistence of SARS-CoV-2 in the Environment and on Surfaces
One of the major questions in the pandemic response has been the contribution of fomite transmission and the persistence of the SARS-CoV-2 virus in the environment and on surfaces. Early reports confirmed that the SARS-CoV-2 virus, much like its predecessors MERS and SARS-CoV-1, did persist on surfaces for significant periods of time, from a few hours (aluminum, surgical gloves, paper) to days (wood, metal, plastic, silicone) (Van Doremalen et al., 2020). One study of several cruise ships that were hard hit by COVID-19 infections showed SARS-CoV-2 RNA present in cabins up to 17 days following disembarkation of all infected travelers, showing that the virus can persist for long periods of time in certain environments, even without a host (Yamagashi et al., 2020). More recent studies have shown that the virus can persist on objects that are commonly used and frequently passed, like money, and cell phone screens, for up to 1 month (Riddell et al., 2020). Importantly, this study also considered the viability of the virus and showed it was able to persist, viable, for this significant period of time on the right material and under the right environmental conditions. This does show the potential risk posed by environmental persistence of SARS-CoV-2 and this risk should be assessed through the initial detection of the virus followed by subsequent disinfection to reduce the risk of transmission. There are still important questions that need to be asked to determine whether the virus is still virulent/infective after these lengths of time, how environmental conditions impact viral infectivity and what viral titers are more common in the built-environment and result in typical fomite transmission. However, it is certain that surface transmission occurs and it is one of the trickier types of transmission to definitively identify as the source of a case since it would commonly exist in outbreak scenarios with many infections occurring within confined spaces and within a short period of time (nursing homes, cruise ships), or during uncontrolled community outbreaks where the source of most transmission events is unidentified.
Asymptomatic and Pre-symptomatic Transmission
One of the many reasons that SARS-CoV-2 is a dangerous virus and highly contagious is due to the relatively high percentage of people who seem to contract the virus but show no symptoms of disease (asymptomatic), exhibit mild symptoms that may not elicit concern and/or are pre-symptomatic, but still shedding viral particles that are infective. The available evidence across a range of populations indicates that asymptomatic and pre-symptomatic patients can test positive for SARS-CoV-2 at rates ranging from 17.9% to 58%. This is highly dependent on the context of the environment. For example, on the Diamond Princess Cruise ship which experienced an outbreak outside of Japan, approximately 58% of those who tested positive for SARS-CoV-2 (712 people) were asymptomatic or pre-symptomatic (CDC EID, 2020). Further, a large scale (>9000 people) testing initiative in Iceland found approximately 50% of the people selected for testing were found to be asymptomatic positive (CNN, 2020). Another study that investigated an outbreak in a skilled nursing facility in Washington State, showed 56% of infected residents were identified as either pre-symptomatic or asymptomatic (Arons et al., 2020).
Using a holistic approach with existing COVID-19 testing tools can help to break transmission chains and mitigate the potential for environmental transmission. Here we propose the use of qRT-PCR testing methodologies to thoroughly assess the risk of COVID-19 and inform reopening plans through a science-guided risk management approach. The goal is to ensure effective risk discovery and disease containment using objective data provided by best-in-class tools. Notably, using environmental surveillance monitoring tools to detect SARS-CoV-2 in the built environment where pre-symptomatic and asymptomatic cases can be discovered days prior to clinical presentation (if at all) means identifying infections and breaking chains of transmission before they turn into outbreaks.
A complete COVID-19 testing strategy should be deployed in the appropriate environment to ensure surveillance is proactive and identifies potential outbreaks before they require mass clinical testing, quarantines and restrictive policies that effectively shutter economic activities and reduce normal societal movements. This begins with comprehensive SARS-CoV-2 testing, including environmental testing that can be used to better guide and inform the more costly and reactive clinical diagnostic tests.
Enhanced Environmental Monitoring for SARS-CoV-2
What is SARS-CoV-2 Environmental Testing?
SARS-CoV-2 environmental monitoring solutions are based on the gold standard qRT-PCR technology that is used to help diagnose COVID-19. The difference is that these environmental tests are not confined to use by healthcare professionals and are designed to put the power of advanced detection technology into the hands of the asset owners who require them the most. Distinct testing workflows enable detection of SARS-CoV-2 on surfaces, air and in wastewater. Combined with clinical diagnostic testing administered by trained health professionals, monitoring the environment for SARS-CoV-2 is an effective tool for early detection and is a useful surveillance tools to assure clients, customers and/or taxpayers that every affordable option is being pursued to ensure their health is a top priority (Figure 2).
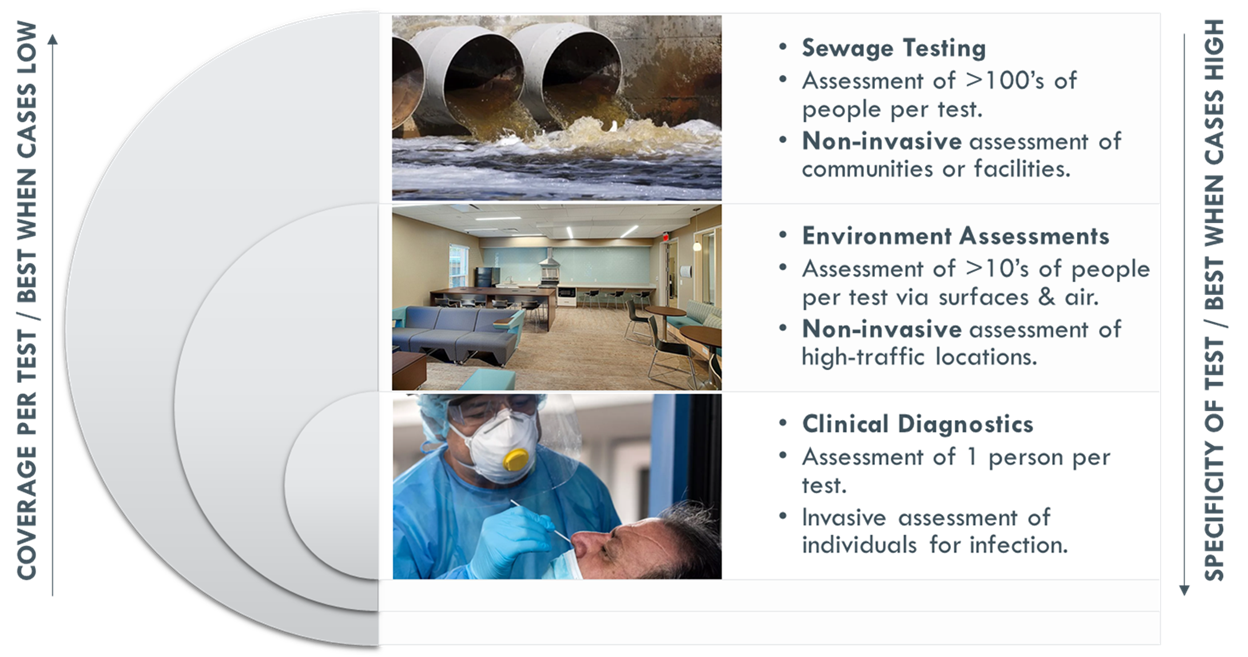
Figure 2: Summary of the complete suite of environmental and diagnostic SARS-CoV-2 testing tools to implement a virus discovery and containment strategy proactively and efficiently
SARS-CoV-2 Surface Detection Workflow
For SARS-CoV-2 surface detection, the most efficient method for field-based monitoring is the Direct method, which is designed for rapid, field-deployable detection in a portable package. The methodology consists of four simple steps:
Step 1: Sample via Surface Swab. A sample is collected using a swab for surface samples and then immediately placed into a tube containing a proprietary testing buffer which inactivates any viable virus and preserves the viral RNA for a short period of time. Samples can be stored in the sample tube for up to 16 hours at ambient temperature, or 72 hours at 4°C.
Step 2: Sample Processing. SARS-CoV-2 is an RNA virus, meaning that its genetic information is encoded in RNA rather than DNA. In this step, RNA is isolated from the preserved sample collected in the previous step using heat treatment. The processed sample is placed in a heat block and treated at 95°C for 10 minutes and then cooled to room temperature.
Step 3: RT-qPCR Assay. The purified RNA is mixed with the provided assay reagents and then placed into a LuminUltra GeneCount® qPCR device for analysis. Inside the reaction tube the viral RNA is reverse-transcribed from RNA into DNA, then small pieces of DNA called primers and probes specifically matching the SARS-CoV-2 virus are used to amplify sections of viral sequence, resulting in a fluorescent signal monitored by the device, which automatically reports results as positive or negative. This assay is based on the latest primers and probes developed by the US Centers for Disease Control (CDC) in March 2020 for detecting SARS-nCoV-2 (CDC-006-00019, Rev: 04).
Step 4: Results Analysis. All data for the run is collected and analyzed in LuminUltra’s GeneCount® software. The results include the qPCR amplification curves with Ct values and interpretation guidelines for the outcomes based on these Ct values. When SARS-CoV-2 is present, even in minute quantities, it will be interpreted as detected. The amount of the virus present can be assessed by observing the amplification curve and Ct value. The lower the Ct value, the higher the amount of SARS-CoV-2 present. If there is no amplification curve (and hence, no Ct value) the virus is not detected. A graph showing typical curves in the software is shown in Figure 3.
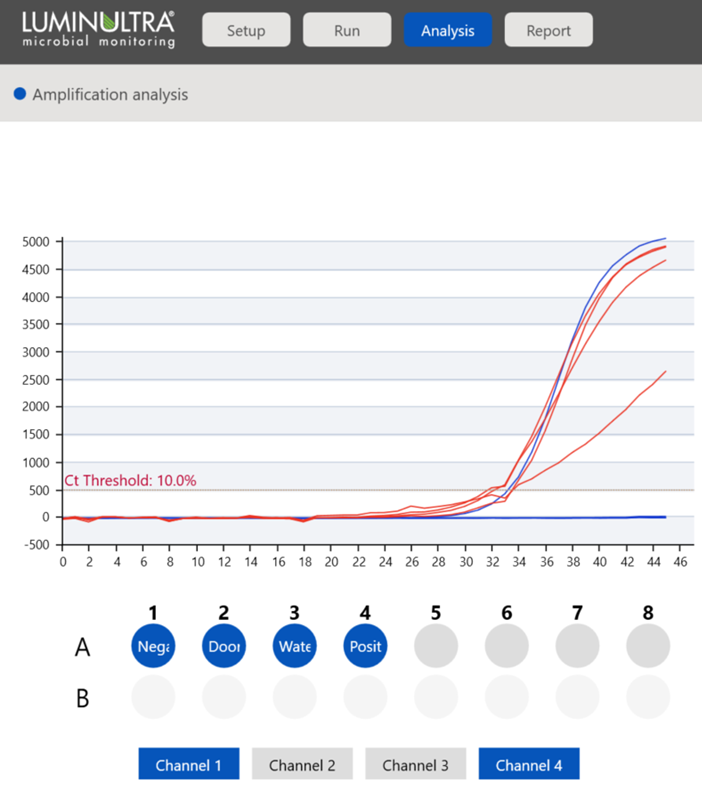
Figure 3: Amplification analysis of qPCR data in LuminUltra’s GeneCount® software platform
The software performs all calculations and analysis for the user, presenting the results in an easy-to-review and understand format as seen in Figure 4.
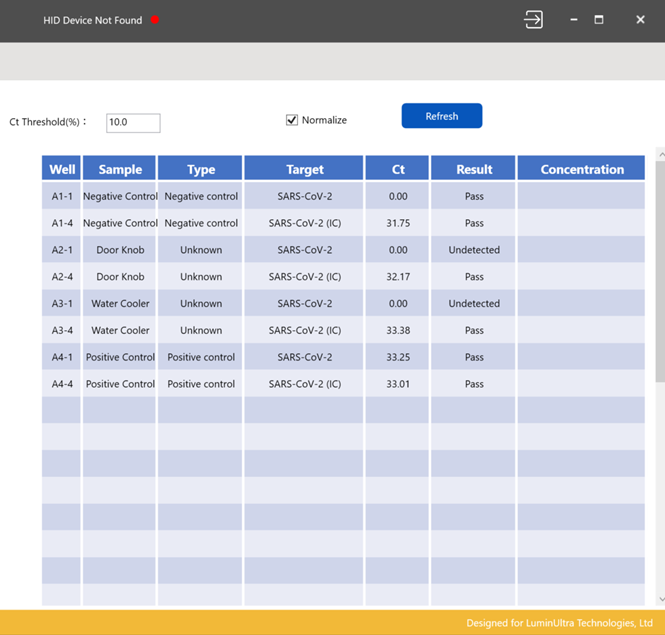
Figure 4: GeneCount® software results output table. Each test run also includes an internal control run in the background to ensure the reaction mechanisms are working as designed
Wastewater Applications:
Monitoring for Community-Level Surveillance
There are several different levels of testing that can be implemented to achieve the goal of reducing COVID-19 disease. From a hierarchical perspective, testing population or community health non-invasively and broadly is at the top of the list for pandemic surveillance. Monitoring wastewater for early detection of viral pathogens, including SARS-CoV-2, has proven to be an effective advanced warning system alerting public health professionals to potential COVID-19 outbreaks up to a week prior to clinical presentation at hospitals (Peccia et al., 2020). This advance warning could mean the difference between a rampant community outbreak requiring strict lockdown implementation or successfully alerting a community to the potential for asymptomatic transmission of the virus through the detection of SARS-CoV-2 in wastewater prior to clinical diagnosis by healthcare professionals. Additionally, if wastewater-detected levels do not match case load numbers reported by public health, there would be indications of potential community and/or asymptomatic transmission that have not yet been identified through community health detection mechanisms. Population-level health data can be determined with daily wastewater tests that get the same level of information as testing hundreds or thousands of individuals, and it is much faster. Wastewater testing provides a holistic assessment of large groups of people without the invasive and costly clinical diagnostic testing model, which represents a much more efficient use of resources in a time when both materials and human resources are in short supply.
Arizona State University applied wastewater testing internally on their campus at the start of the semester in September with the hope of catching potential outbreaks and guiding contract tracing efforts to contain the virus (Maya 2020). The deployment of this testing allowed university officials to monitor the health of all residential buildings on campus through testing wastewater at strategic locations outside of building collection systems, making each test specific to a building or residence. The testing allowed the university to detect the SARS-CoV-2 virus in a building where no clinical diagnosis had been made, as the students had just arrived on campus and all residents had tested negative prior to being allowed entry. The positive wastewater test allowed university officials to immediately conduct targeted clinical testing for residents of the building, which ended up identifying two individuals who were asymptomatically shedding the virus. These individuals and were immediately isolated from the general population to avert a potential outbreak among high contact individuals susceptible to infection and transmission, and follow-up wastewater tests revealed no further virus load.
Surface Applications: Monitoring for High-Risk Areas
While wastewater monitoring provides the broadest measure of a community’s health through population-wide detection of viral shedding, surface detection drills one step further to building-specific health and allows monitoring of high-risk areas without reliance on individual health metrics. Surface detection of SARS-CoV-2 can be used to assess risk in community settings, such as office buildings, schools, nursing homes, airports, public transit and any public infrastructure that is critical to be open for the economy to function at a high level.
Monitoring high traffic areas and high frequency touch points within those heavily trafficked areas for SARS-CoV-2 is an integral part of a holistic testing program to identify transmission risk prior to individual disease epidemiology would show up in a clinical context. The strategy for program implementation is highly dependent on the local disease situation and the intended goals. Some common programs where surface-monitoring can provide value include:
- Simple surveillance-mode (low risk)
- Cleaning efficacy confirmation (medium risk)
- Outbreak monitoring (high risk)
During surveillance-mode, disease pressure would generally be expected to be very low and local rules would be considered successful at reducing the spread of COVID-19. In this case, there would be very little to no known community transmission of the virus and all known cases can be attributed to close contact of a known positive, which typically occurs after importation of the coronavirus through travel to known hotspots. A surveillance program in this case would provide much needed confirmation that the public health measures that have been implemented in a jurisdiction are indeed effective at containing the virus and there are no breaches in the measures deployed. If a breach is detected, follow-up measures can be quickly implemented to mitigate the breach, including conducting contact tracing and ensuring those at risk are tested and isolated as appropriate. Effective surveillance would include monitoring public locations where large gatherings or groups of people are required to come into close contact for employment, educational or recreational purposes, such as office buildings, universities, or sporting events.
Facilities that house the most vulnerable populations such as long-term care homes, assisted-living homes and nursing homes, would greatly benefit from additional measures to prevent viral entry into the environment. Schools (K-12) also represent high-risk environments for transmission of the SARS-CoV-2 virus due to the close proximity of attendees and the risk of asymptomatic transmission amongst young people. Highly durable and robust cleaning programs must be implemented to reduce possible contamination and transfer events in these high-risk environments. Proper cleaning regimes are integral to disease suppression in these settings and the only way to confirm that cleaning programs are effective is to measure reduction of the virus presence through cleaning. Surface detection programs will provide this assessment and confirm when a cleaned surface is safe for other residents and/or attendees to be present on a daily basis and providing actionable measures of how effective cleaning programs are in the first place. In addition, if a viral breach is detected, the area can be immediately deep-cleaned and deemed virus-free for the next cohort of residents or attendees. In addition, contact tracing can begin immediately to isolate the potentially-impacted persons and prevent any further undiscovered transmission of the virus, effectively breaking the transmission chains.
Conclusions
SARS-CoV-2 is a viral pathogen unlike any the modern global populace has ever seen, with heavy human casualties primarily due to a high reproductive rate (R0), comparatively high case fatality rate (CFR), and high prevalence of spread through asymptomatic and pre-symptomatic means. A holistic approach can be used to proactively monitor for the virus in the environment to preserve clinical testing for the most vulnerable and impacted populations. Using the right tool to find viral hotspots and mitigate the risk of transmission through aggressive cleaning, disinfection, and contact tracing efforts to identify potential carriers and ensure they are tested and isolated, is the most effective method to control COVID-19 spread.
Opening society safely so that it remains open starts by casting the widest net possible to reduce COVID-19 exposure; utilizing wastewater monitoring as an early warning surveillance system for overall population-level health is the most effective use of resources. Monitoring can be accomplished at the municipal or city level and is particularly effective when disease pressure in a given area is not high and is under control. Continuous monitoring at the wastewater level will ensure any breaches of containment can be caught and sequestered quickly. Wastewater testing can also be used to trace an event to a more granular level, including specific neighborhoods, facilities, or parts of a complex. Continuous monitoring of specific high-risk segments like cruise ships, sporting facilities, nursing homes, shopping complexes, office buildings, universities or schools would also be appropriate uses for the technology. Drilling down to the next resolution level, surface level-testing can be used to monitor environments proactively that have been shown to act as vehicles for super spreader events, primarily highly-populated, enclosed spaces with poor ventilation. Finally, when these surveillance methods alert authorities to the potential for increased disease pressure, further tracing to the source of the outbreak can be applied to guide clinical diagnostic testing, contact tracing and the appropriate isolation schemes. Using science-guided decision making with the best available tools, it is possible to return to some form of normal economic operation and keep our people safe.
References
Alcendor, D.J. (2020). Racial Disparities-Associated COVID-19 Mortality among Minority Populations in the US. Journal of Clinical Medicine, 9(8):2442.
Arons, M.M. , K.M. Hatfield, S.C. Reddy, A. Kimball, A. James, J.R. Jacobs, J. Taylor, K. Spicer, A.C. Bardossy,L.P. Oakley, S. Tanwar, J.W. Dyal, J. Harney, Z. Chisty, J.M. Bell, M. Methner, P. Paul, C.M. Carlson,H.P. McLaughlin, N. Thornburg, S. Tong, A. Tamin, Y. Tao, A. Uehara, J. Harcourt, S. Clark, C. Brostrom-Smith,L.C. Page, M. Kay, J. Lewis, P. Montgomery, N.D. Stone, T.A. Clark, M.A. Honein, J.S. Duchin, and J.A. Jernigan. (2020). Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility May 28, 2020. N Engl J Med, 382:2081-2090 DOI: 10.1056/NEJMoa2008457
CDC Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission. (Updated Oct. 05, 2020). https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html
Epidemiology of COVID-19 Outbreak on Cruise Ship Quarantined at Yokohama, Japan. (February 2020). Emerging Infectious Diseases, 26(11), 2591-2597. https://dx.doi.org/10.3201/eid2611.201165
Godri Pollitt KJ, Peccia J, Ko AI, et al. (2020). COVID-19 vulnerability: the potential impact of genetic susceptibility and airborne transmission. Hum Genomics, 14(1):17. Published 2020 May 12. doi:10.1186/s40246-020-00267-3
John, T. (2020). Iceland Lab’s Testing Suggests 50% of Coronavirus Cases Have No Symptoms. CNN. April 03, 2020. https://www.cnn.com/2020/04/01/europe/iceland-testing-coronavirus-intl/index.html
Maya, A. (2020). A Secret Weapon in the Fight against COVID-19 Oct. 13, 2020. https://www.waterworld.com/wastewater/article/14184342/a-secret-weapon-in-the-fight-against-covid19
Moore JT, Pilkington W, Kumar D. (2020). Diseases with health disparities as drivers of COVID-19 outcome [published online ahead of print, 2020 Aug 20]. J Cell Mol Med. doi:10.1111/jcmm.15599
Morawska, L and Cao, J. (2020). Airborne transmission of SARS-CoV-2: The world should face the reality. Environment International, 139: 105730. https://doi.org/10.1016/j.envint.2020.105730
Moriarty LF, Plucinski MM, Marston BJ, et al. (2020). Public Health Responses to COVID-19 Outbreaks on Cruise Ships — Worldwide, February–March 2020. MMWR Morb Mortal Wkly Rep 69:347-352. DOI: http://dx.doi.org/10.15585/mmwr.mm6912e3
Otter, J.A., Donskey, C., Yezli, S., Douthwaite, S., Goldenberg, S.D., and Weber, D.J. (2016). Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. Journal of Hospital Infection: 92 (3) 235-250 https://doi.org/10.1016/j.jhin.2015.08.027
Peccia, J., Zulli, A., Brackney, D.E. et al. (2020). Measurement of SARS-CoV-2 RNA in wastewater tracks community infection dynamics. Nat Biotechnol 38, 1164–1167. https://doi.org/10.1038/s41587-020-0684-z
Riddell, S., Goldie, S., Hill, A. et al. (2020). The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol J 17, 145 https://doi.org/10.1186/s12985-020-01418-7
Roncha, R. (2020). What Countries did right and wrong in responding to the pandemic. CBC News. June 22, 2020. https://www.cbc.ca/news/canada/covid-19-coronavirus-pandemic-countries-response-1.5617898’
Sheikh A, Sheikh A, Sheikh Z, Dhami S, Sridhar D. (2020). What’s the way out? Potential exit strategies from the COVID-19 lockdown. J Glob Health. 10(1):010370. doi:10.7189/jogh.10.010370
Sweetland, H.S. (2020). There Are Sensible Ways to Reopen a Country. Then There’s America’s Approach. May 14, 2020. https://time.com/5836607/reopening-risks-coronavirus/
The Editors. (2020). Dying in a Leadership Vacuum. Oct. 08, 2020. New England Journal of Medicine; 383:1479-1480 https://www.nejm.org/doi/full/10.1056/NEJMe2029812
TIME Magazine. The Best Global Responses to COVID-19 Pandemic. June 12, 2020. https://time.com/5851633/best-global-responses-covid-19/
van Doremalen N, Bushmaker T, Morris DH, et al. (2020). Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 382: 1564-1567 DOI: 10.1056/NEJMc2004973
Yamagishi T, Ohnishi M, Matsunaga N, et al. (2020). Environmental Sampling for Severe Acute Respiratory Syndrome Coronavirus 2 During a COVID-19 Outbreak on the Diamond Princess Cruise Ship. J Infect Dis., 222(7):1098-1102. doi:10.1093/infdis/jiaa437