Abstract
I often refer to antimicrobial resistance as the slow-burning pandemic that continues to spread like a smoldering wildfire – picture a large expanding, ignored sustained bed of coals that continues to make global progress by sparking fires around the world. Antibiotic and antimicrobial resistance is everyone’s problem. The Centers for Disease Control and Prevention state that each year in the United States, at least 2.8 million people are infected with antibiotic-resistant microbes, and more than 35,000 die as a result.
The UN Ad hoc Interagency Coordinating Group on Antimicrobial Resistance report warns us that, without action, drug-resistant diseases could cause 10 million deaths each year by 2050. Furthermore, damage to the economy as catastrophic as the 2008-2009 global financial crisis can be expected. By 2030, antimicrobial resistance could force up to 24 million people into extreme poverty. At least 700,000 people die each year due to drug-resistant diseases, including 230,000 people who die from multidrug-resistant tuberculosis. More and more common diseases, including respiratory tract infections, sexually transmitted infections, and urinary tract infections, are untreatable; lifesaving medical procedures are becoming much riskier, and our food systems are increasingly precarious.
How can we help? What can those of us who work in public health and healthcare do to help curb this global emergency? The following commentary will discuss recent research and insight regarding how laboratories can play a critical role in reducing antimicrobial resistance.
Main Article – Commentary
Antibiotic resistance (AR) and overall antimicrobial resistance (AMR) is a complex issue that has currently reached a dangerous tipping point. Although frequently associated with antibiotics, AMR is not a phenomenon exclusive to bacteria. Other pathogens including viruses, fungi and protozoa also exhibit this ability to respond to antimicrobials, further demonstrating the dangerous scope of AMR in infectious diseases. Therefore, AMR represents a massive public health concern for pathogens ranging from influenza, to Pseudomonas aeruginosa (bacteria), to Plasmodium falciparum (the malaria parasite), to Candida (fungi). This puts a tremendous burden on healthcare providers and healthcare infrastructure, particularly in developing countries where resources can already be scarce.1
Whether one is discussing AR or AMR, together they represent a slow-burning global emergency. The World Health Organization (WHO), Centers for Disease Control and Prevention, and other similar agencies have predicted that AMR could lead to an economic impact of $100 trillion dollars and cause 10 million deaths annually by 2050 if the world does not take action. If this occurs, AMR will lead the world in mortality over longtime leaders like cancer and other health related conditions.
The Misuse of Antimicrobials
The efficacy of antimicrobials, particularly antibiotics, has led to their overuse and misuse. If honest, all of us have been in a situation where we utilize an antimicrobial / antibiotic without a prescription or without a confirmatory medical laboratory test and antibiotic susceptibility test. Whenever antibiotics are used, a selective pressure is applied, and the bacteria that escape that pressure can then proliferate or transfer the resistance gene; this can occur when antibiotics are taken during a virus infection. Antibiotics are meant to target bacteria, and therefore, have little-to-no effect when it comes to viral infections. Thus, the virus pathogen will be unaffected, but the bacteria existing in the patient’s body are being put through an antibacterial bottleneck in which only the strongest survive.2 The same scenario can be true when antibiotics are incorrectly used during an allergy or for other non-bacterial agents. Examples of this could include a fungal infection (like athlete’s foot) or infection with a protozoan (like malaria). Therefore, not only can taking antibiotics select for resistant bacterial populations, but the treatment will also do nothing for the patient suffering from a non-bacterial infection. This can then lead to the rise of AMR bacterial pathogens. Ultimately, whenever it is possible, antibiotics should be prescribed only for a bacterial infection. AMR has also contributed largely to the issue of healthcare and community associated infections. It is critical that physicians and others with the authority to prescribe antibiotics should do so based on a confirmatory medical laboratory tests and antibiotic susceptibility panels.3,4
Ultimately, the driver of antimicrobial resistance regarding prescribing of antibiotics empirically or improperly arrives front and center as one of the world’s most dangerous health issues. The interaction between a number of healthcare professionals – physicians, pharmacists, nurses, and medical laboratorians – must be one of open communication that encourages antibiotic stewardship. Recently, I discussed the specific importance of antimicrobial stewardship with respect to the pharmacy and medical laboratory professionals.5 Each of us in these different healthcare professions have an obligation to attack AMR synergistically in a variety of ways.
Nudging – Can Selective Reporting Help?
In an April 2021 research study, Langford et al. conclude that laboratory reporting of antibiotic susceptibility results for urine cultures is associated with empirical and directed prescribing of the reported antibiotics. Laboratories can play an important role in guiding appropriate antibiotic selection for urinary indications.6 Briefly, after a patient specimen is identified as a bacterial pathogen, the medical laboratory / clinical microbiology professional will most often perform an antibiotic susceptibility test (AST) on the pathogen. Testing determines the potential effectiveness of specific antibiotics on the bacteria and/or determines if the bacteria have developed resistance to certain antibiotics. Used properly, the AST results help select the drug(s) that will likely be most effective in treating an infection.
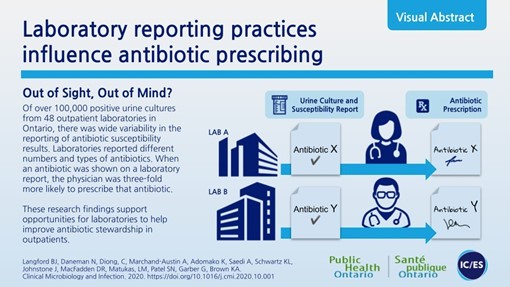
Figure 1. Medical laboratories (microbiology) can augment antibiotic stewardship via selective reporting (nudging) practices. Permission to use image from Langford BJ, May 27, 2021.
This research study has important and practical findings for antibiotic stewardship programs (ASP). Nudging is a term used to describe the concept of modifying choice architecture to augment decision-making, without introducing incentives or inhibiting the personal decision of the physician (or other decision maker.)7 Research is providing evidence that nudging is a promising intervention in the microbiology and medical laboratory.8, 9 Selective reporting via nudging is a process whereby only certain culture and antibiotic susceptibility results are reported back to the clinician; the strategy aims to help guide appropriate antimicrobial prescribing. Selective reporting can take multiple forms, ranging from not reporting any susceptibility results at all to reporting only first-line antibiotics or agents with lower risks of adverse events. While national and international guidelines recommend the use of selective reporting, specific reporting policies are at the discretion of individual laboratories, resulting in a high degree of variability.6,8
the microbiology laboratory can be highly influential in antibiotic prescribing choices
Ultimately, the goal of selective reporting via nudging can influence how a physician does or does not select and/or utilize a particular antibiotic. Langford’s findings6 confirm their hypothesis that there is in fact laboratory variability in selective reporting which influences antibiotic prescribing decisions. There were approximately 3-fold odds of directed antibiotic prescribing when that antibiotic agent was listed on the susceptibility report. There was also an association between laboratory antibiotic susceptibility reporting and prescribing in the empirical window. This suggests that the microbiology laboratory can be highly influential in antibiotic prescribing choices, even when the prescriber is making decisions in the absence of a urine culture result (empirical or syndromic decisions).

Figure 2. Improving antibiotic prescribing in hospitals. Source: CDC Vital Signs, 2014.
Microbiology Laboratories are Essential in Antimicrobial Stewardship
The CDC’s Key Activities and Roles for Microbiology Laboratory Staff in Antibiotic Stewardship Programs outline the ways in which microbiology laboratory staff can impact antibiotic stewardship programs. The following areas are highlighted in the Core Elements of Hospital Antibiotic Stewardship where microbiology staff should provide input.
- Hospital Leadership Commitment – Integrate microbiology laboratory staff into the functions of the antibiotic stewardship program; their expertise is important in the areas of diagnostic stewardship, development of antibiograms to support optimal antibiotic use, the introduction of new diagnostic tests into the laboratory, the implementation of new antibiotic susceptibility testing interpretative criteria, and education of clinicians on laboratory testing practices.
- Accountability – Appoint a leader or co-leaders, such as a physician and pharmacist, responsible for program management and outcomes
- Pharmacy Expertise (previously “Drug Expertise”) – Appoint a pharmacist; ideally as the co-leader of the stewardship program, to lead implementation efforts to improve antibiotic use.
- Action – (1) Prospective Audit and Feedback. (2) Regularly review the way AST is performed in the laboratory, the drugs tested, interpretation, and communication of results.
- Tracking: Facilitate use of Antimicrobial Resistance (AR) Option in CDC’s National Healthcare Safety Network (NHSN) – (1) Work with hospital leadership, in-house information systems technology, electronic health record systems, or third-party AR surveillance systems to enroll and successfully submit data to the NHSN AR Option. (2) Facilities are encouraged to complete the AR Option data validation. Antimicrobial Resistance (AR) Option Data Validation [PDF – 10 pages] (https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/aur/ar-validation-508.pdf ) upon initial setup and implementation as well as on an annual basis or when undergoing a change in vendor system.
- Reporting: Antibiotic Susceptibility (AST) Reporting – At least annually, update institution antibiograms following published guidance in the M39 CLSI
- Education – (1) Promote education and communication between the laboratory and clinicians about test characteristics (e.g., test performance, expected turn-around-time, etc.). (2) Teach staff about best practices in specimen collection. (3) Educate clinicians how to interpret test reports, including understanding report language used, such as categorical interpretations and understanding the principles behind selective reporting and how to contact the laboratory if questions arise regarding additional drug susceptibility results.
For a complete description of this CDC document, which was updated in August 2020, please visit the online publication.
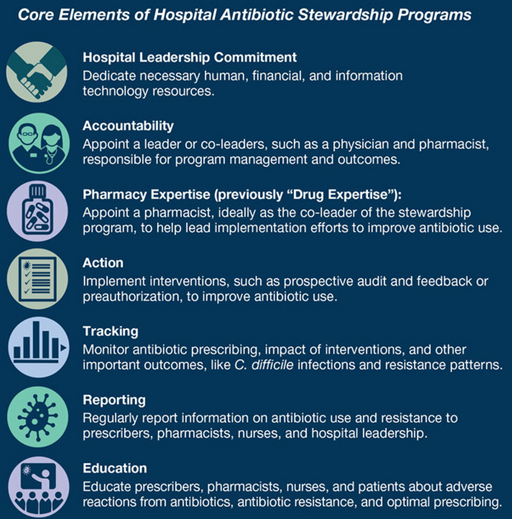
Figure 3. The Core Elements of Hospital Antibiotic Stewardship Programs: 2019. Source: CDC images.
Three Keys for the Microbiology / Medical Laboratory in Antimicrobial Stewardship
When one boils AR / AMR down to the most common denominator, an American Association of Clinical Chemistry publication does an effective job of explaining the role of the laboratory. Three main keys are discussed:
(1) Antibiogram Reporting – Clinical microbiology laboratories conduct surveillance on local antimicrobial resistance trends among microbial pathogens. The collection, organization, and communication of resistance data culminates in the creation of an antibiogram. Antibiograms provide critical information to ASPs and prescribing physicians on institutional susceptibility patterns.
(2) Patient-Specific Information – Laboratories provide patient-specific information by identifying microbial pathogens and performing antimicrobial susceptibility testing. This information is necessary so that empiric antimicrobial therapy can be narrowed appropriately.
(3) Specimen and Reporting Quality – Laboratory guidelines, policies, and procedures that ensure high-quality specimen collection and processing have an important role in limiting unnecessary antimicrobial use.
Lastly, the ongoing and growing development of rapid diagnostics (e.g. MALDI-TOF, PNA-FISH, qPCR, NGS, and other multiplex nucleic acid assays) will continue to offer powerful discriminatory methods for not only pathogen identification but also genes that may confer resistance to antimicrobial drugs. It will be critical for the experts on laboratory testing (medical laboratory professionals) to be at the table for test selection and proper interpretation to aid physicians, pharmacists, and other healthcare professionals. Another important tool for healthcare / hospitals to utilize will be the newly created Doctor of Clinical Laboratory Science (DCLS). The DCLS will be the future of Diagnostic Management Teams and laboratory test utilization at the intersection of open communication with the entire healthcare team, including physicians.
Final Thoughts
In recent publications10-15, I have discussed the overall critical importance of the medical laboratory. Most people, including some in healthcare, do not understand who performs your medical laboratory tests for COVID-19 or any other test. If you answered “my doctor” or “my nurse” or “a robot”, you would be completely wrong.
To put it bluntly, your life is in the hands of medical laboratory professionals. We perform an estimated 13 billion laboratory tests in the United States each year; that means laboratory testing is the single highest-volume medical activity in the lives of Americans.
Why should you care? Those 13 billion tests help drive approximately two-thirds of all medical decisions made by your doctor and other health care professionals from cradle to grave. There are only 337,800 practicing medical laboratory professionals for a population of just over 330 million people in the U.S. It is critical that all healthcare professionals understand the critical role laboratory medicine plays in not only antibiotic / antimicrobial resistance and antibiotic stewardship decisions, but in all patient health decisions.
References
- Rohde, R.E. & McNamara, R.P. Globalization and Antimicrobial Resistance: A Moving Target. Clin Lab Sci, 2018; DOI: http://clsjournal.ascls.org/content/early/2018/06/04/ascls.118.000489
- Low D. Reducing antibiotic use in influenza: challenges and rewards. Clinical Microbiology and Infection. 2008;14(4):298-306. https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(14)62800-7/fulltext
- Rohde RE, Felkner M, Reagan J, Mitchell AH, Tille P. Healthcare-Associated Infections (HAI): The Perfect Storm has Arrived. Clinical laboratory science. 2016. p. 28-31. http://clsjournal.ascls.org/content/29/1/28
- Rohde, R.E. Two Laboratory Tests you must Demand – Advice from MRSA Survivors and a Scientist. InfectionControl.tips https://infectioncontrol.tips/2016/01/11/2labtests-mrsa/
- Rohde, R.E. Without Good Public Health Strategy, The Coronavirus Pandemic Could Make Antimicrobial Resistance Worse. September 16, 2020. Accessed May 27, 2021 from https://www.forbes.com/sites/coronavirusfrontlines/2020/09/16/without-good-public-health-strategy-the-coronavirus-pandemic-could-make-antimicrobial-resistance-worse/?sh=4db82cde1016
- J. Langford, Nick Daneman, Christina Diong, et. al. Antibiotic susceptibility reporting and association with antibiotic prescribing: a cohort study. Clinical Microbiology and Infection, Volume 27, Issue 4, 2021, pp. 568-575, ISSN 1198-743X, https://doi.org/10.1016/j.cmi.2020.10.001
- H. Thaler, C.R. Sunstein. Nudge: improving decisions about health, wealth, and happiness. Yale University Press, New Haven (2008), p. 293. https://books.google.com/books?hl=en&lr=&id=NGA9DwAAQBAJ&oi=fnd&pg=PR7&ots=CsK5ISWpcM&sig=ObzG3fuMpAK_yUqj-vrDUOQBUhY#v=onepage&q&f=false
- J. Langford, E. Leung, R. Haj, M. McIntyre, L.R. Taggart, K.A. Brown, et al. Nudging in MicroBiology laboratory evaluation (NIMBLE): a scoping review. Infect Contr Hosp Epidemiol, 40 (2019), pp. 1400-1406. https://pubmed.ncbi.nlm.nih.gov/31679535/
- Katchanov, S. Kluge, C.R. MacKenzie, A.J. Kaasch. “Nudging” in microbiological reports: a strategy to improve prescribing. Infection, 45 (2017), pp. 123-127. https://link.springer.com/content/pdf/10.1007/s15010-016-0938-3.pdf
- Rohde R.E. To Beat Covid Variants, The U.S. Must Do More To Find Them. Forbes, Coronavirus Frontlines, Healthcare, April 21, 2021. https://www.forbes.com/sites/coronavirusfrontlines/2021/04/21/to-beat-covid-variants-the-us-must-do-more-to-find-them/?sh=4dff7de720b1
- Rohde R.E. Who is doing all those COVID-19 tests? Why you should care about medical laboratory professionals. The Conversation. December 14, 2020. https://theconversation.com/who-is-doing-all-those-covid-19-tests-why-you-should-care-about-medical-laboratory-professionals-151725
- Rohde R.E. What Happens When Laboratory Tests Fail? Microbiologics Blog, November 4, 2020. https://blog.microbiologics.com/what-happens-when-laboratory-tests-fail/?fbclid=IwAR08YTALt_YEisH9B5UO0JnDF2C7ZzY0jUhqmxM3GkYCCSqFS6QeFT9yxp0
- Rohde R.E. Beating Pandemics Like COVID-19 Requires More Medical Laboratory Professionals, This Virologist Explains. Forbes, Coronavirus Frontlines, Healthcare. April 23, 2020. https://www.forbes.com/sites/coronavirusfrontlines/2020/04/22/beating-pandemics-like-covid-19-requires-more-medical-laboratory-professionals-this-virologist-explains/?fbclid=IwAR1M3suIlaPqYS7U1N7i_zT13SFOBu4CmrJPLJ0SK_SCGp7T6ZIpG12vI7I#48f108366e32
- Rohde R.E. Celebrating Medical Laboratory Professionals – We Save Lives Every Day! American Society for Microbiology, Bugs and Drugs, Invited online article, April 23, 2020. https://asm.org/Articles/2020/April/Celebrating-Medical-Laboratory-Professionals-We
- Rohde R.E. #PublicHealth Matters ALL the time to EVERYONE – Public Health Thank You Day #PHTYD19. Invited online article for tips, November 25, 2019. https://infectioncontrol.tips/2019/11/25/publichealth-matters-all-the-time-to-everyone-public-health-thank-you-day-phtyd19/