Peer Reviewed
Disclaimer: The authors of this report and InfectionControl.tips declare no conflict of interest with the following critical evaluation and research.
Editors Note: Correct Order of Authors is as follows: Andrew Duong, Murray Cohen, Dr. Jason Davies, Dr. Michael Ackerman
Acknowledgements: The authors wish to express their grateful appreciation to Thomas H. Taylor, P.E. and Rik Heller for assistance with data management and interpretation.
Abstract
People often overestimate their own healthiness and doing so can have negative consequences when employees decide to continue to work while sick. Depending on the work environment and the illness, a sick employee can infect coworkers, customers, students, patients, and the general public. The introduction of a screening system to prevent infected individuals from spreading pathogens could have a real, positive impact on public health by mandating employee absenteeism during illness. In this study, it was found that most subjects believe their own health to be better than average; and that they are less susceptible to illness than others. Measurement of the subjects’ temperatures using the WelloStationX and the tympanic ear thermometer demonstrated that most subjects were within normal body temperature ranges, and that there was much agreement between both instruments (mean temperatures of 36.9˚C and 36.7˚C for the WelloStationX and ear thermometer, respectively). However, there was greater intra-measurement variability for the ear thermometer compared to the WelloStationX (SD=0.165 and 0.037, respectively). The adoption of a new technology to provide high-throughput, self service temperature screening of individuals in public spaces could dramatically reduce the spread of disease.
Introduction
In 2003, the SARS outbreak represented a global crisis that brought to attention the need for an efficient screening program to evaluate patient and traveller risk. Through concerted efforts, a number of technologies were enrolled in multiple capacities to quickly monitor the public for one of the first indicators of illness, people with elevated temperatures (Bitar, Goubar, & Desencios, 2009). The spread of SARS quickly crossed borders and thus such technologies were rolled out in airports to reduce the risk of global spread of the disease (Bitar et al., 2009).
Body temperature has traditionally been measured using thermometers requiring contact with the patient and one health care worker to administer.. Early thermometers required the thermometer to be in contact with mucosal layers or armpits, and required a long contact time (Center for Disease Control, 2014). The development of novel non-contact thermometers has reduced the time required to determine a patient’s temperature, as well as reducing the transfer of potential pathogens (Davie & Amoore, 2010). Non-contract, infrared skin thermometers are easy to use and can quickly evaluate a subject’s temperature, but can be extremely variable in their readings (Lahiri, Bagavathiappan, Jayakumar, & Philip, 2012). Tympanic thermometers are infrared thermometers (typically inserted the ear) and are generally considered more accurate than other non-contact thermometers (Canadian Agency for Drugs and Technologies in Health, 2014).
Thermal imaging was employed in airports during the SARS outbreak and has the benefit of being contact-free, while allowing for rapid screening of individuals without a potential transfer of pathogens (Ring & Ammer, 2012). Thermal imaging can be accurate for subjects, but is complicated due to calibration issues and the subtleties of body temperature and the distance between measuring device and subject (which can span several metres) (Cho & Yoon, 2014; Ring & Ammer, 2012; Shu et al., 2005). Consequently, higher temperature or fever thresholds are set to avoid false positives. Current technologies, such as the WelloStationX have taken advantage of new sensor technology, combined with advanced software, to accurately diagnose fevers and are the latest innovations so as to facilitate outbreak management.
The ability of infectious diseases to spread will be accelerated as infected people continue to work, travel, and interact with the public. This will occur despite the person exhibiting common symptoms, such as a high fever. It has been previously shown that patients are not necessarily the best judges of their own health and will continue to work while exhibiting symptoms of illness (Sen, 2002).
In this study we evaluate the WelloStationX and FDA-approved ear thermometer (FDA# K060006) for accuracy, and also determine subject perception of their own health.
Methods
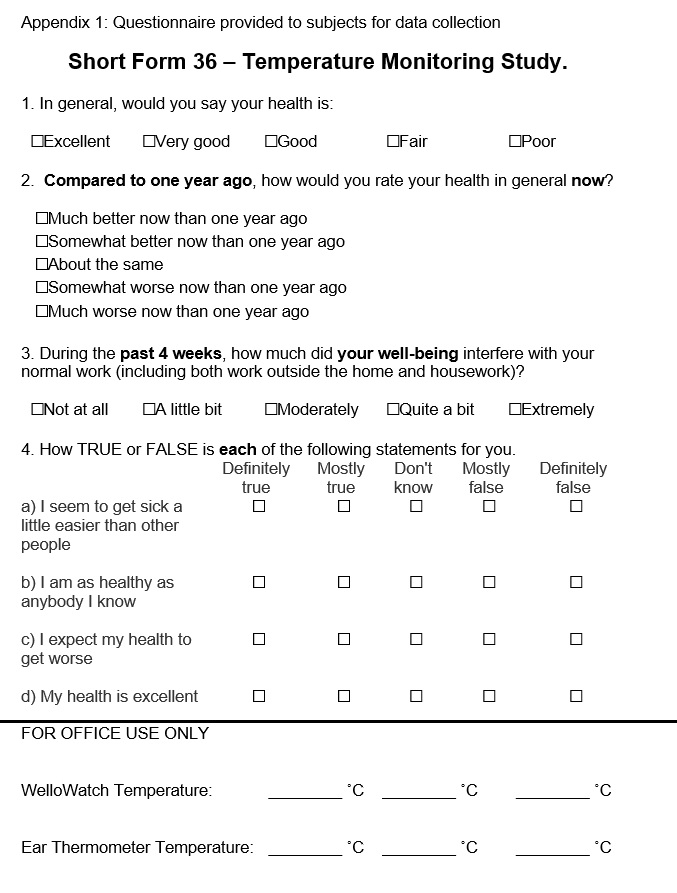
Subjects were recruited at the University of Buffalo and Niagara University. Study participants were all volunteers who received no renumeration for their participation. Consented subjects were asked to fill out a short questionnaire that is abbreviated from the validated SF-36 form (appendix 1). Following the survey, the subjects’ temperatures were measured using a tympanic ear thermometer (Braun Thermoscan 5), as well as the WelloStationX temperature monitoring system in triplicate. In the pilot phase, temperatures were only recorded once on each instrument; in the subsequent project phase each subjects’ temperatures were recorded twice on each instrument.
Descriptive statistics were calculated using Microsoft Excel. Due to subject variability in body temperature, standard deviation was calculated based on the triplicate data and reported as average standard deviation.
Results
A total of 126 subjects were recruited at the University of Buffalo and Niagara University. Subjects were predominantly students and healthcare workers, but also included salespeople and librarians (n=8). The majority of subjects reported that their health was “very good,” followed by “good.” The majority of respondents (60.3%) reported that their health had not changed since last year. Forty-one percent of subjects stated that their health was much better or slightly better than it was a year ago. Only 7.1% of subjects stated a slight decline in health within the past year.
In terms of wellbeing, 68.9% of respondents stated that their wellbeing had not interfered with regular daily activities within the past two weeks (including work outside the home and housework). The majority of statements regarding their own changing health indicated that most people believe they get sick less than their peer group, are healthier than their peer group, expect to get healthier in the future, and are in excellent health overall (77.0%, 69.8%, 61.9%, and 86.5%, respectively).
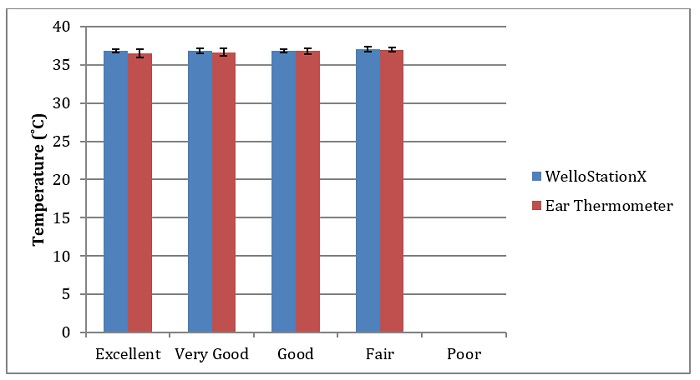
The temperatures of 58 pilot subjects were measured only once. The temperatures of 68 additional subjects were recorded in triplicate. The average body temperature range (from the triplicate measurements) was between 36.3˚C to 37.5˚C and 35.5˚C to 37.5˚C using the WelloStationX and the tympanic ear thermometer, respectively. On average, the subjects’ temperature were 36.9˚C (standard deviation, SD = 0.03) and 36.8˚C (SD = 0.166) for the WelloStationX and ear thermometer, respectively. The temperatures are shown in Figure 1. The R-squared (R2) value for the data was 0.274. On average, the temperature of the WelloStationX was 0.17 degrees higher than that of the ear thermometer. There was no relationship observed between subject wellbeing and temperature (Figure 2, p >0.05).
Figure 1: Correspondence of WelloStationX temperature readings with ear thermometer temperatures. Each data point indicates one subject and their respective average temperature reading using each instrument.
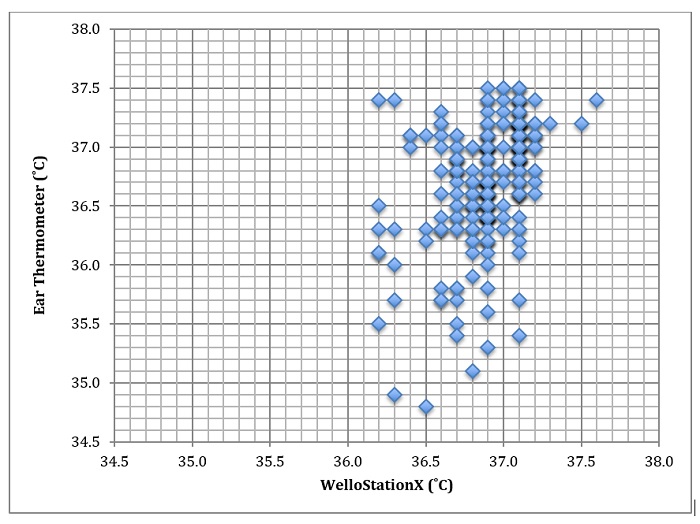
Figure 2: Subject wellbeing and observed temperatures.
Discussion
In this study, the personal perception of health and its relatedness to body temperature was evaluated. One hundred and twenty six subjects were recruited from the University of Buffalo and Niagara University. Most subjects reported that they were in good to very good health. The temperatures of the subjects ranged from 35.5˚C to 37.5˚C. On average, there was substantial agreement between the temperature measured by the WelloStationX and the tympanic ear thermometer. The WelloStationX and ear thermometer only differed by 0.17˚C on average. It was noted that there was more intra-subject variance in ear thermometer readings compared to the WelloStationX.
Questionnaire respondents
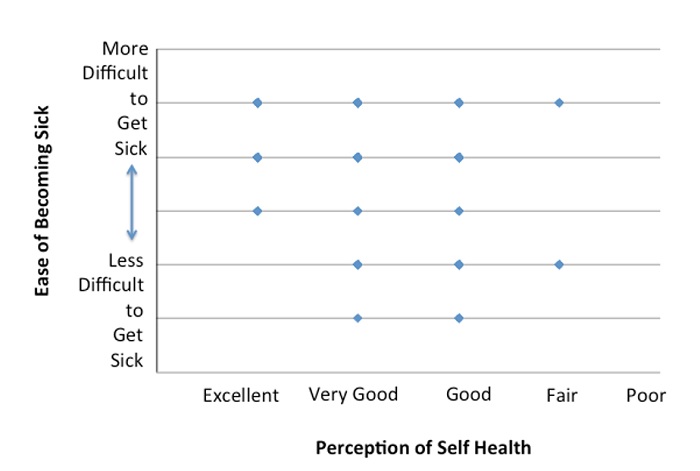
A person’s viewpoint of their own health can be influenced by a number of factors. In this study, most respondents stated that they were in good or very good health. In previous studies, it was found that well-designed questionnaires (such as the SF36 questionnaire) were predictive in identifying the number of times that a person would seek a physician’s services in a year. Subjects who rated themselves as healthier were less likely to go to a doctor (Miilunpalo, Vuori, Oja, Pasanen, & Urponen, 1997). However, another article stated that self perceptions can be inaccurate, as people tend to misrepresent themselves on self-reported questionnaires (Sen, 2002). Depending on the measure to determine health of the subject, both instances can be true. On the questionnaire, there was no relationship between how healthy a subject thought they were and how often they got sick (Figure 3).
Figure 3: Subjects’ perceptions of health and their ease of becoming sick.
Temperature measurements
Overall, the measurements from the WelloStationX were in agreement with the measurements from the ear thermometer. There was a negligible difference of only 0.17˚C, on average. There was a higher standard deviation in the measurements using the ear thermometer compared to the WelloStationX (0.17 and 0.03, respectively). The number of outliers (temperature outside the normal range) using the ear thermometer was more frequent. Higher intra-subject variation within temperature readings using the ear thermometer was also observed. Both instruments were well within the range of accuracy as determined by the FDA, and can be used interchangeably for the measurement of body temperatures.
Tympanic ear thermometers have been extensively evaluated for their accuracy and are in general agreement with the temperatures recorded by rectal thermometers (Craig, Lancaster, Taylor, Williamson, & Smyth, 2002; Yaron, Lowenstein, & Koziol-McLain, 1995). However, similar to our findings, some studies have found that tympanic thermometers have greater variability which can be attributed to the person administering the exam (Amoateng-Adjepong, Del Mundo, & Manthous, 1999; Yaron et al., 1995). Small variances in how far an ear thermometer is placed into the ear canal and the length of time that a thermometer is used for can impact an accurate reading. Regardless, these variances are considered minimal and are generally not a concern for healthcare professionals.
Improving Technologies for New Uses
The WelloStationX and tympanic ear thermometer were both consistent and accurate in their ability to measure subject temperatures. Despite the increased variance associated with user error regarding the ear thermometer, ear thermometers remain an affordable and accurate method to measure a patient’s temperature.
The WelloStationX allows for rapid, contactless (non-invasive) high volume screening of many subjects through a simple 10 second scan of their forehead. Since the WelloStationX does not require any patient contact, the potential spread of pathogens to both healthcare workers and subsequent patients is reduced (Heller, 2017). Its rapid measurement time allows for screening of more individuals in the same time period.
Our results show that personal perceptions are skewed towards better health than is the case, which is of concern to workplaces. An employee may believe they are suitably healthy for work, but may harbour an infection. If an employee is ill and still chooses to work, they are putting coworkers at risk for an infection. These effects were seen during the SARS outbreak in Singapore. It was found that a large proportion of the public entering the country reported no illness, despite having a fever or other SARS-like symptoms (Goh et al., 2006). A simple scan upon entry can identify employees who require additional assessment of their health status before they can expose coworkers. This removes the burden from workers, who are sometimes required to prove their illness before being granted a day of sick leave. This is especially important in public places such as airports, hospitals, and food service, as having sick employees at work is a concern for public health and outbreaks of infectious diseases (Heller, 2017).
Conclusions
The WelloStationX and tympanic ear thermometer were both found to be quite accurate for the measurement of a subject’s body temperature. The ear thermometer had greater variance in temperature measurements and thus, the WelloStationX was more precise for temperature monitoring. The majority of subjects responded that they were in good health, but also believed that their health was better than average. This suggests that respondents may have skewed perceptions of their own health and that the use of routine temperature screening would be more useful for places of employment to reduce the number of sick workers entering the workplace, thus reducing the spread of disease.
References
Amoateng-Adjepong, Y., Del Mundo, J., & Manthous, C. A. (1999). Accuracy of an Infrared Tympanic Thermometer. Chest, 115(4), 1002–1005.
Bitar, D., Goubar, A., & Desencios, J. (2009). International travels and fever screening during epidemics: a literature review on the effectiveness and potential use of non-contact infrared thermometers, 14(6), 1–5.
Canadian Agency for Drugs and Technologies in Health. (2014). Non-Contact Thermometers for Detecting Fever: A Review of Clinical Effectiveness. CADTH Rapid Response Reports, 11, 1–38.
Center for Disease Control (2014). Non-contact temperature measurement devices: considerations for use in port of entry screening activities.Retrieved December 19, 2016, from http://wwwnc.cdc.gov/travel/pdf/ebola-non-contact-temperature-measurementguidance.pdf
Cho, K. S., & Yoon, J. (2014). Fever Screening and Detection of Febrile Arrivals at an International Airport in Korea: Association among Self-reported Fever, Infrared Thermal Camera Scanning, and Tympanic Temperature. Epidemiology and Health, 36, e2014004.
Craig, J. V, Lancaster, G. A., Taylor, S., Williamson, P. R., & Smyth, R. L. (2002). Infrared ear thermometry compared with rectal thermometry in children: a systematic review. The Lancet, 360(9333), 603–609.
Davie, A., & Amoore, J. (2010). Best practice in the measurement of body temperature. Nursing Standard, 24(42), 42–49.
Goh, K.-T., Cutter, J., Heng, B.-H., Ma, S., Koh, B. K. W., Kwok, C., … Chew, S.-K. (2006). Epidemiology and control of SARS in Singapore. Annals of the Academy of Medicine, Singapore, 35(5), 301–16.
Heller, R. (2017). The Need for Rapid Contagion Screening. InfectionControl.tips, 2, 1–3. Retrieved from https://infectioncontrol.tips/2017/02/21/need-for-rapid-contagion-screening/
Lahiri, B. B., Bagavathiappan, S., Jayakumar, T., & Philip, J. (2012). Medical applications of infrared thermography: A review. Infrared Physics & Technology, 55(4), 221–235.
Miilunpalo, S., Vuori, I., Oja, P., Pasanen, M., & Urponen, H. (1997). Self-rated health status as a health measure: The predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. Journal of Clinical Epidemiology, 50(5), 517–528.
Ring, E. F. J., & Ammer, K. (2012). Infrared thermal imaging in medicine. Physiological Measurement, 33(3), R33–R46.
Samaan, G., Patel, M., Spencer, J., & Roberts, L. (2004). Border screening for SARS in Australia: what has been learnt? The Medical Journal of Australia, 180(5), 220–3.
Sen, A. (2002). Health: perception versus observation. BMJ (Clinical Research Ed.), 324(7342), 860–1.
Shu, P.-Y., Chien, L.-J., Chang, S.-F., Su, C.-L., Kuo, Y.-C., Liao, T.-L., … Huang, J.-H. (2005). Fever Screening at Airports and Imported Dengue. Emerging Infectious Diseases, 11(3), 460–462.
Yaron, M., Lowenstein, S. R., & Koziol-McLain, J. (1995). Measuring the accuracy of the infrared tympanic thermometer: Correlation does not signify agreement. The Journal of Emergency Medicine, 13(5), 617–621.
Appendix













We are thrilled to know IC.tips field study found the welloStation to be a powerful solution for improving workplace health using our revolutionary approach – self-service fever screening. This is awesome to me because I’ve “caught germs at work,” and now I know welloStation can prevent this. This is a momentous “step” in our journey to improve workplace health for everyone!
[…] platform provided evidence-based science for several remarkable innovations. Our work on Rapid Temperature Screening for Workplace Health involved a real-world subject study that involved IRB/Ethics approval and engagement within multiple […]
[…] View the full study on InfectionControl.tips: https://infectioncontrol.tips/2017/06/12/rapid-temperature-screening-for-workplace-health/ […]
[…] Our recent study showed that adoption of this new technology to provide high-throughput, self-service temperature screening of individuals in public spaces could dramatically reduce the spread of disease. […]
[…] Rapid Temperature Screening for Workplace Health Real world subject study that involved IRB/Ethics approval and engagement within multiple hospital environments. Our team developed the methods, wrote the IRB submission, conducted the study, authored the paper, submitted for peer review and published the findings.Other notable deliverables included: Distribution, Marketing, Deep Dive Podcast interview, Showcase events in Buffalo, Dallas and Toronto, Trials and Pilots, UK, USA and Canada conference support.View Study: https://infectioncontrol.tips/2017/06/12/rapid-temperature-screening-for-workplace-health/ […]