As the world continues to navigate the ever-changing waters of the COVID-19 pandemic, one message has been consistent: wash your hands. Even before COVID-19, we have long known that hand hygiene is the most effective way to prevent infections. Now, more than ever, the public is being reminded, and in some cases required, to perform hand hygiene more frequently – from hand sanitizer in building lobbies to wipes for grocery carts.
Once a member of the community becomes hospitalized, patient access to hand hygiene supplies is inconsistent, even in today’s COVID-19 world. Emphasis on hand hygiene in the hospital setting is centered on healthcare workers. Patient hand hygiene is an obvious component of infection prevention but one that is usually overlooked and rarely stressed (Wallace, 2015).
Earlier this year, just a week before the United States went into quarantine, a group of nursing students at the University of California in Irvine completed a project that addressed the issue of patient hand hygiene in hospitals and sheds light on how we can make measurable improvements.
For the process improvement project, the students specifically wanted to understand patients’: (1) access to hand hygiene products; and (2) awareness of the importance of patient hand hygiene while hospitalized.
To start, the students did extensive research on how poor hand hygiene increases the risk of hospital-acquired infections (HAIs). Their findings reveal a stark reality: there is a domino effect when patients do not clean their hands enough. The risk of infections spreading rises throughout a hospital; patients who acquire infections have a longer length of stay which can resources and increase costs; and, in the worst cases, hospital acquired infections lead to patient deaths.
Improving patient hand hygiene will help decrease patient deaths and reduce hospital costs
More than 2.5 million people are affected by HAIs each year in the United States with approximately 90,000 deaths. To put this in perspective: more patients die from HAIs each year than from breast and prostate cancer combined. Hospitals spend about $15,000 per HAI resulting in about $4.5 billion in costs annually (Fox, 2015). Improving patient hand hygiene will help decrease patient deaths and reduce hospital costs. So, what is the best way to do this? As many on the frontlines of healthcare will attest, making sure patients clean their hands is not as straightforward or easy as it sounds. Hospital nurses and staff are already overworked, and most hospitals do not have standardized processes to address the issue of patient hand hygiene.
The UCI nursing students decided to take on this challenge and set three primary goals for this project: (1) to increase accessibility to hand hygiene supplies; (2) to increase patient hand hygiene knowledge; and (3) to increase patient compliance to hand hygiene protocols. Using concepts from theories of communication, power and empowerment, leadership and patient-centered care, the nursing students developed a pretest / post-test project design. Patients who were awake, alert, English speaking and without contraindications to hand sanitizer use were selected from a Burn Intensive Care Unit and an Orthopedics Unit. All patients selected for the project were immobile.
GOAL #1: Increase Accessibility to Hand Hygiene Supplies
The students researched potential ways to provide patients with access to hand sanitizer and selected a patient bedside caddy called Fitsi. Fitsi, shown in Figure 1, attaches to bed rails, stands upright on its own, rotates to accommodate different bed angles, is made with an antimicrobial agent called Micro- Bloc S, and is recyclable. By having Fitsi at their bedside, patients were able to access hand sanitizer without the help of a caregiver.
GOAL #2: Increase Patient Hand Hygiene Knowledge
Patient hand hygiene education was provided as part of the pretest. Patients were then surveyed using six questions related to infection prevention and hand hygiene. The questions were asked: (1) before receiving hand sanitizer in a Fitsi; and (2) one day after having access to a bedside caddy with hand hygiene supplies.
GOAL #3: Increase Patient Compliance to Hand Hygiene
For this goal, students aimed to increase hand hygiene compliance through a combination of improving patients’ understanding of the importance of patient hand hygiene and making it easier to clean their hands by providing them with accessible hand hygiene supplies in a bedside caddy. As is often the case in healthcare, there is no single solution to the problem of patient hand hygiene. As a result, the students designed the project to show how a holistic approach is needed to really drive change in patient behavior. Patient hand hygiene is a problem that requires a human-centered solution.
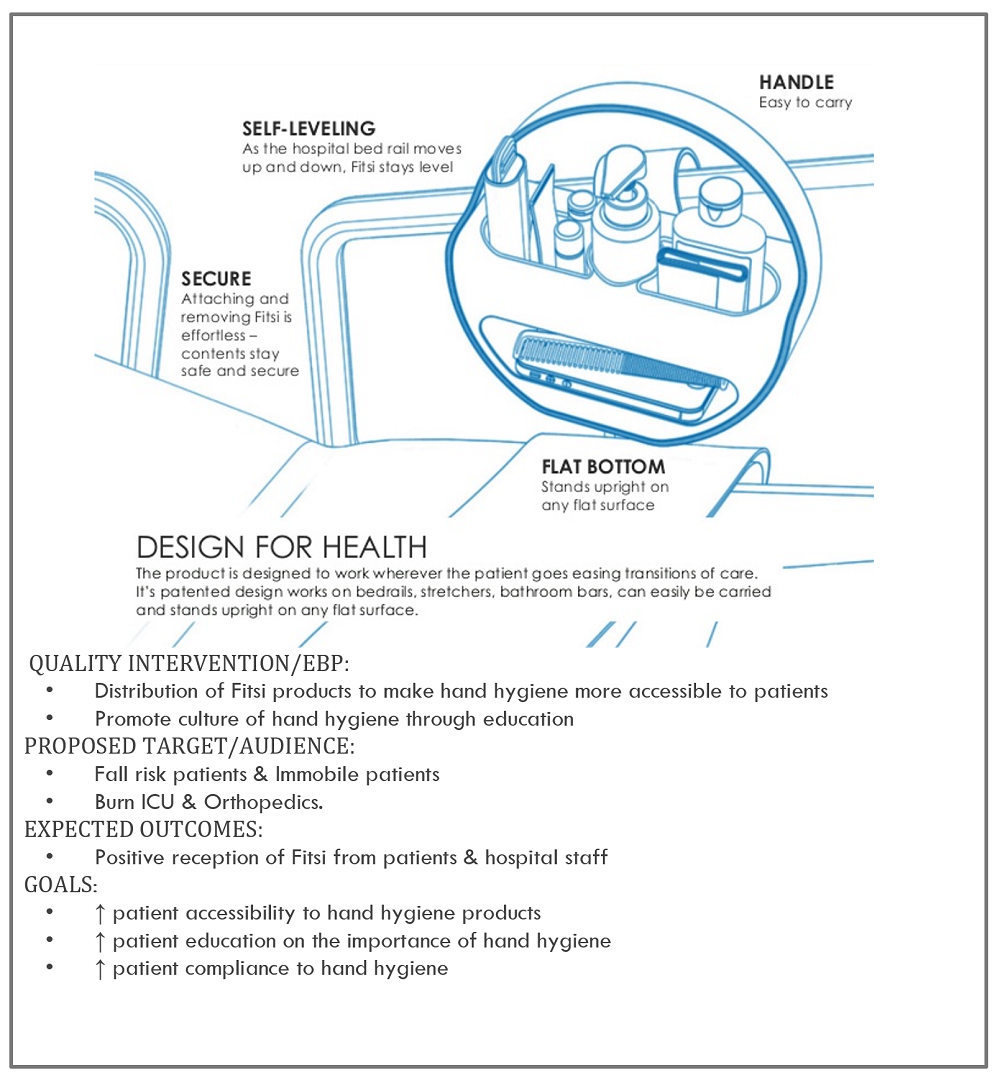
Figure 1. Overview of Quality Improvement Project with description of the Fitsi bedside caddy.
The results from the students’ project are positive and build a case for greater patient hand hygiene education and improving access to hand sanitizer for patients, particularly those who are immobile.
Prior to receiving the education and better access, many patients answered that the best way to prevent infections was to use antibiotics or to clean an area. Figure 2 demonstrates that patient education increased awareness of hand washing being the most effective way to prevent infection by 44.97%. Patient education also improved by 38.62% from pretest to posttest patients’ knowing that the most important part of hand hygiene is friction, as shown in Table 1.
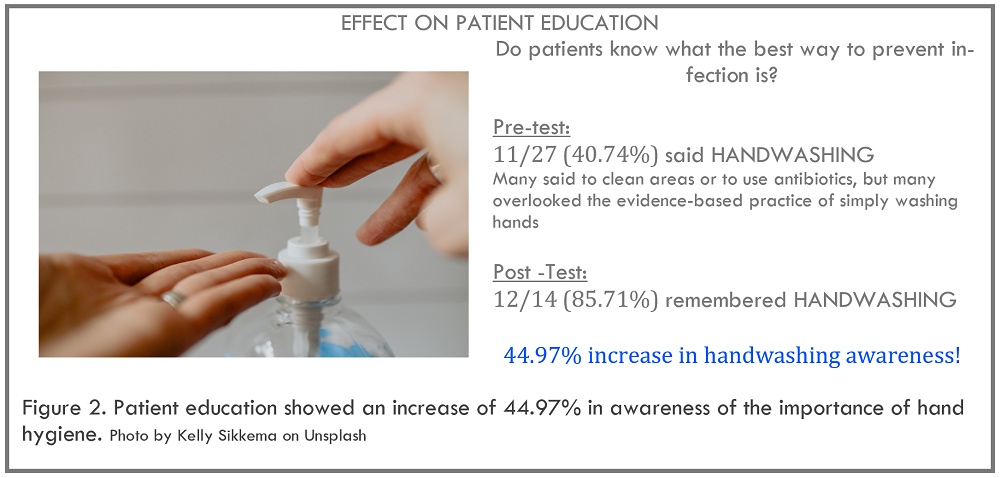
Figure 2
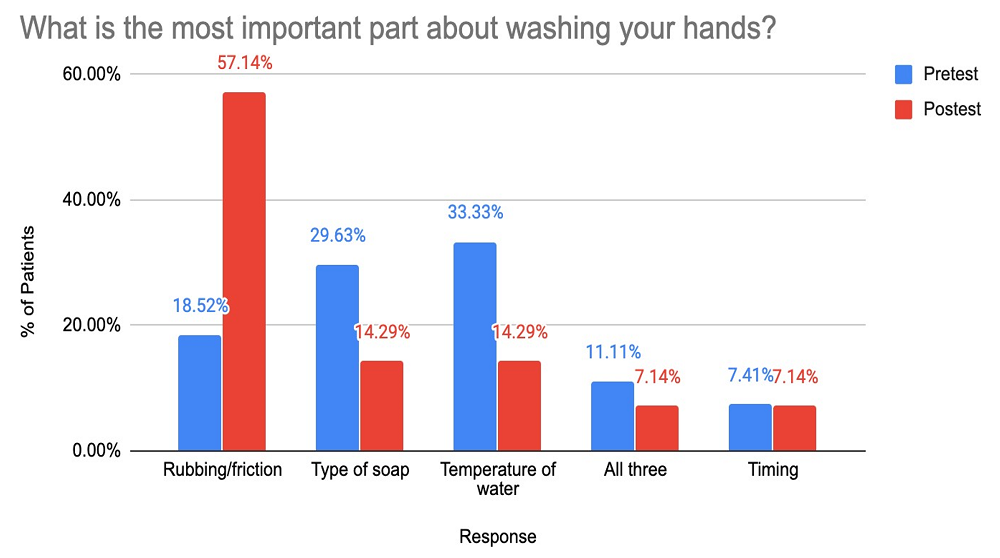
Table 1. Patient education demonstrated an improvement of 38.62% in retention of friction / rubbing as major element of hand hygiene effectiveness
Providing patients with easy access to hand sanitizer proved to be a positive intervention. A 15.87% decrease in difficulty when cleaning hands was realized. Table 2 shows there was a 49.21% increase in patients reporting no barriers to hand washing, and hand hygiene compliance improved by 15.31% as patients reported washing their hands four times a day or more once they had hand sanitizer at their bedside, as shown in Table 3.
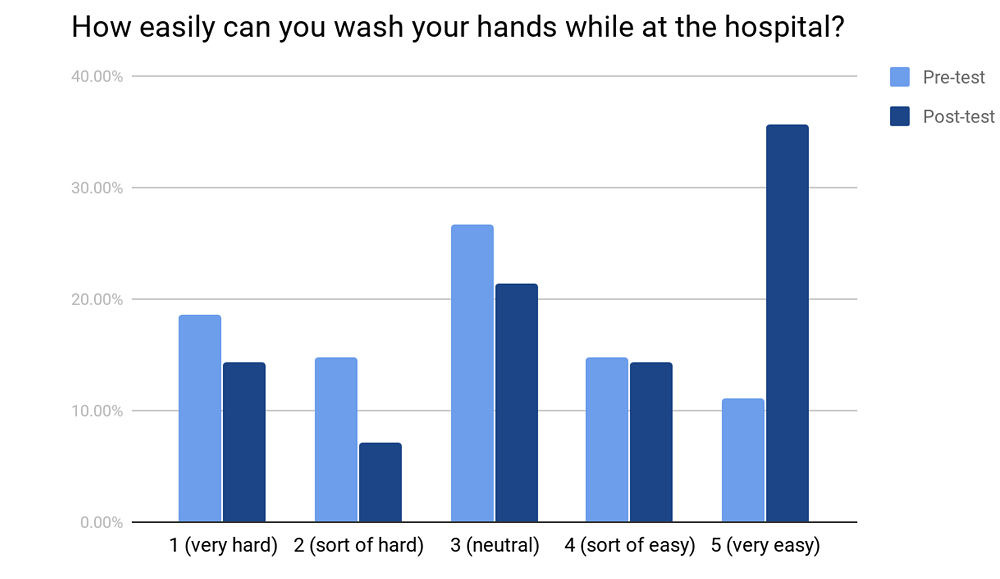
Table 2. After receiving accessible hand sanitizer, a 49.21% increase in patients reporting no barriers to hand hygiene.
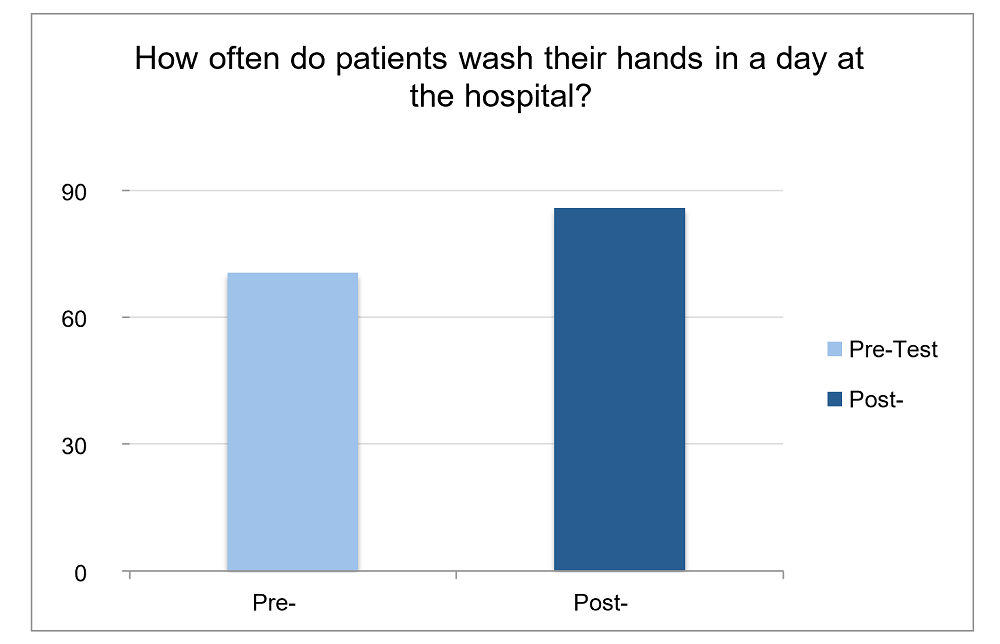
Table 3. Hand hygiene compliance improved by 15.31% with hand sanitizer in a beside caddy
References
Fox, C., Wavra, T., Drake, D. A., Mulligan, D., Bennett, Y. P., Nelson, C., Kirkwood, P., … Bader, M. K. (2015). Use of a patient hand hygiene protocol to reduce hospital-acquired infections and improve nurses’ hand washing. American Journal of Critical Care, 24, 3, 216-224.
Wallace, N. (2015, December 9). Patient Hand Hygiene: The missing link in preventing Hospital Acquired Infections? Retrieved from https://www.infectiocontroltips.