Updated: Tuesday February 2, 2016
Abstract:
Background: Vector-borne diseases are defined primarily by how they are spread. While many insects and arachnids can spread a diverse variety of microbes (bacteria, virus, protozoa, etc.), the mosquito is particularly notorious for its efficient spread of blood borne agents. Currently, a “new” (not really) arbovirus known as Zika has made the headlines in the U.S. On January 11, 2016, Texas health officials confirmed the latest case of imported Zika in one patient who recently traveled to Latin America and subsequently exhibited characteristic symptoms including fever, rash and joint pain. Areas of Texas, like in some other states in the southern U.S., are home to two species of Aedes mosquitoes capable of transmitting Zika; however, there are no known cases of local transmission of the disease so far in the U.S. mainland. Zika follows a long history of other mosquito transmitted viruses, like dengue, West Nile virus, and chikungunya.
Significance: As with any “new” emerging infectious disease, it is critical for global, national, state, and local public health officials to report correct information in regards to any significant health threat to the general public. One doesn’t need to look that far back to see how the introduction of Ebola in to the U.S. created unnecessary panic in many people. While Zika, like other arboviruses, does pose some health threats and risks, we should be careful to not create public health hysteria by adding any material for sensationalized headlines. Facts, along with common sense advice and concern, are all that is needed in this latest “threat” to our shores. Those of us in the realm of public health and medical arenas should offer a consistent message, one of instruction and caution, but not of panic.
Main Article:
Zika has arrived in North America. If you live in Texas where a case was confirmed, you have no doubt read the headlines and have read of the dangers of the disease and its link to birth defects. However, the truth is that the recent confirmed case was contracted in Latin America, not Texas; and the correlation between Zika and birth defects is being studied for causation, but has not been confirmed. The media may be exaggerating the threat of Zika to garner the attention of their audience, but such tactics are not helpful and may put undue stress on the public health system.
The media may be exaggerating the threat of Zika
Such hysteria and sensationalism is often stirred up when a new infectious disease is introduced to the public. In 1999, while working as a public health microbiologist and molecular epidemiologist for the Texas Department of State Health Services (DSHS), I began hearing about the first cases of West Nile virus (WNV) entering the U.S. in New York.1 I can still see the headlines and news reports of imminent disaster for all mankind. This occurrence of WNV in the U.S. and its impact on society made an early, deep and lasting impression on my professional outlook with regards to where science, particularly infectious diseases, intersected with the general public. It also directly impacted my understanding of how the popular press and media can affect public health in my life personally. By this, I mean, how it impacted my actual work day and those of my colleagues in public health laboratories and programs at DSHS, CDC, and across the U.S.
In those days at the DSHS laboratory, we were very busy with two rabies epizootics in Texas.2-4 We were receiving up to 100 animal specimens to be necropsied for rabies testing and it kept us very busy in our unit of about 10 laboratory professionals. Once WNV made its first index case in Texas, we were overwhelmed with birds, equine specimens, and mosquito pools for WNV testing; the sheer number of samples were in the thousands! We were truly overwhelmed. This is not uncommon. Each time there is a new flu strain, foodborne outbreak, or “new” scary disease (WNV, SARS, anthrax, plague, Ebola, etc.), the public health systems in this country are overwhelmed. Likewise, those of us in healthcare know all too well how quickly our emergency rooms and other acute care areas can be overwhelmed with the latest news story.
In most cases, the WNV “outbreaks” have become endemic and consistent and the risk is low for the majority of people. It’s more likely that you will die in a typical car accident than from WNV or Eblola.5 Often what is most dangerous is right under our noses, like MRSA infections or other HAIs.
It’s a double-edged sword:
we must get the correct information out to the public and healthcare, but we must be cognizant and protective of the message.
Those in the public health and medical community, as well as those reporting the news, must cooperate to properly convey potential threats while taking care not to sensationalize the story and cause hysteria. It’s a double-edged sword: we must get the correct information out to the public and healthcare, but we must be cognizant and protective of the message.
Zika – Who are you?
Zika fever is a mosquito-borne viral disease caused by Zika virus (ZIKV), consisting of mild fever, rash (mostly maculo-papular), headaches, arthralgia, myalgia, asthenia, and non-purulent conjunctivitis, occurring about three to twelve days after the mosquito vector bite. One out of four people may develop symptoms, but in those who are affected, the disease is usually mild with symptoms that can last between two and seven days. Its clinical manifestation is often similar to dengue; another a mosquito-borne illness.6,7 Severe disease from ZIKV requiring hospitalization is uncommon. A possible link between ZIKV infection in pregnant women and subsequent birth defects is being investigated in Brazil.8 ZIKV is in the Flavivirus genus of viruses in the family Flaviviridae. This genus includes the WNV, dengue virus, tick-borne encephalitis virus, yellow fever virus, zika virus and several other viruses which may cause encephalitis.
ZIKV outbreaks have occurred prior to the recent case in Harris County (Houston, Texas) in areas of Africa, Southeast Asia, the Pacific Islands and South America. Because the Aedes species mosquitoes that spread ZIKV virus are found throughout the world, it is likely that outbreaks will spread to new countries. In December 2015, Puerto Rico reported its first confirmed ZIKV virus case. Locally transmitted Zika has not been reported elsewhere in the United States, but cases of Zika have been reported in returning travelers.
A total of 14 Zika cases in the U.S occurred before 2014, according to CDC. Since 2015, eight additional cases have occurred via U.S. travelers to endemic areas returning home. Currently, that means 22 total cases have been observed in the U.S., but the CDC is still receiving specimens for ZIKV testing from U.S. travelers who became ill in 2015 or 2016.7 Like my experiences in Texas, an epidemiologic spike in cases will occur when one starts “looking for the virus more actively.” Those of us in public health see this when surveillance becomes active versus passive.
On January 11, 2016, Texas (USA) health officials confirmed the latest case of imported Zika in Harris County in a patient who had recently traveled to Latin America and subsequently exhibited characteristic symptoms including fever, rash and joint pain. Areas of Texas, like in some other states in the southern U.S., are home to two species of Aedes mosquitoes capable of transmitting Zika, but there are no cases of local transmission of the disease in the U.S. mainland so far. The approximate distributions of the two Aedes species are shown in the below maps.
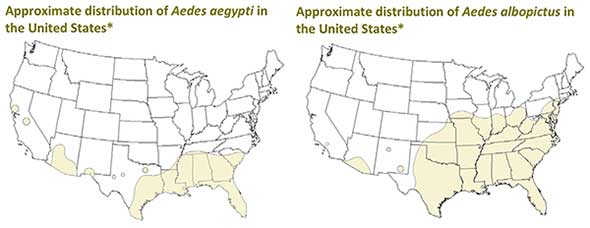
CDC National Center for Emerging Zoonotic and Infectious Diseases
Currently, there is no vaccine to prevent or medicine to treat ZIKV infections. Travelers can protect themselves from this disease by taking steps to prevent mosquito bites. When traveling to countries where ZIKV (or other mosquito-borne viruses are endemic or have been reported), use insect repellent, wear long sleeves and pants, and stay in places with air conditioning or that use window and door screens. These are historically tried and true common sense preventative measures.

Countries that have past or current evidence of ZIKV transmission
(as of December 2015)
Practice:
Perspective, common sense and calm, rational decision-making in consultation with medical and public health authorities / experts to possible ZIKV cases should be the rule not the exception. News outlets, the popular media, and journalists should adhere to the highest standards of reporting cases accurately with, where possible, step-by-step plans and information for the general public. The general public should always practice a level of precaution with respect to any new microbial introduction in one’s home country and locality. If you have a reason to suspect a ZIKV infection (or any other infection for that matter), you should discuss it with your physician and healthcare team. You should not become an overnight graduate of “Google Medical School” and decide your diagnosis. All suspicious cases of any infections should be confirmed by a laboratory diagnosis. Please, follow the science and research on these issues, not the latest hysteria.
Final Thoughts:
ZIKV, like many of its friends and cousins (WNV, dengue, and chikungunya) will continue to make their way to our shores and others. The Pan American Health Organization (part of the World Health Organization) says only one in four people infected with Zika will develop symptoms and those symptoms will typically be mild.
Research is currently under way on the possibility of any mother-to-child transmission of the virus and its effects on babies. Pregnant women in general, and particularly those who develop symptoms of Zika virus infection, should be informed and more closely monitored by health providers. The rest of us should pay attention, listen to the proper authorities, and go about our normal lives. Perspective, with proper caution, is the right way to respond.
As always, access to accurate information, preventative measures and diagnostic tools will be the key to controlling Zika and any other infectious disease to come along. And, remember this: Thank your unsung public health workers, medical laboratorians, physicians, nurses, and other healthcare professionals out there in the trenches working to protect you every day, even when it’s not in the headlines!
Update: February 1, 2016
The World Health Organization has declared a ‘Public Health Emergency of International Concern’ due to the temporal association of Zika virus and an increase in the number of children born with microcephaly in Brazil. Making this declaration will mobilize people and resources to:
• improve the surveillance and reporting of the presence of Zika virus and incidences of microcephaly
• intensify research into whether or not there is a causative link between the virus and the neurologic condition
• take aggressive measures to control the mosquito population and reduce infection with Zika virus
So now is it time to panic? No. WHO is taking a proactive, ‘better safe than sorry’ approach to Zika. By bringing global attention to the temporal association between Zika and microcephaly, pregnant women know to take precautions and doctors know to look for the correlation if problems do arise during pregnancy or at childbirth. Except for (possibly) pregnant women, Zika remains a virus with mild symptoms and no known long-term complications.
References:
- Sejvar, James J. West Nile Virus: An Historical Overview. Ochsner J. 2003 Summer-Autumn; 5(3): 6–10.
- Sidwa, T., R.E. Rohde et al. Evaluation of Oral Rabies Vaccination Programs for control of rabies epizootics in coyotes and gray foxes: 1995-2003. J Am Vet Med Assoc 2005;227(5):785-792.
- Rohde, R.E. May, 2008. Controlling Rabies at its Source: The Texas Experience – Oral Rabies Vaccination Program. ASCLS Today, 22(5), 14-15.
- Wilson, P.J. & Rohde, R.E. 8 things you may not know about rabies but should. Elsevier Connect, September 28, 2015. http://www.elsevier.com/connect/8-things-you-may-not-know-about-rabies-but-should Accessed January 9, 2016.
- Griffith, James T. and Rohde, R.E. Ebola: Implications for the Clinical Laboratory. December 2014; Clin Lab Sci :1-6. See: http://www.ascls.org/images/publications/journals/Ebola_virus_manuscript.pdf Accessed January 13, 2016.
- Zika Virus Infection. http://www.paho.org/hq/index.php?option=com_topics&view=article&id=427&Itemid=41484 Accessed January 13, 2016.
- Zika Virus. http://www.cdc.gov/zika/index.html Accessed January 13, 2016.
- Possible association between Zika virus and microcephaly. http://www.cdc.gov/zika/pdfs/possible-association-between-zika-virus-and-microcephaly.pdf Accessed January 13, 2016.
- Zika Primer: What is Zika Virus Fever? https://infectioncontrol.tips/2015/12/05/zika-primer-what-is-zika-virus-fever/ Accessed January 13, 2016.













[…] Infection Control Tips: Zika Cases Confirmed in North America: Time to Panic? […]
[…] Zika follows a long history of other mosquito transmitted viruses, like dengue, West Nile virus, and chikungunya. […]
[…] from R. Rohde article: Zika Cases Confirmed in North America: Time to Panic?Accessed February 3, […]
[…] A paper by Dr. Rodney Rohde, adjunct professor of biology, was selected for the Zika Virus Resource Center by the online database and academic publisher Elsevier. The paper “Zika Cases Confirmed in North America: Time to Panic?” examines the cause of the virus and appropriate measures for prevention. Read the paper. […]
[…] Rohde, Rodney E. (2016, January 14). Zika Cases Confirmed in North America: Time to Panic? [Article on InfectionControl.tips]. Accessed February 11, 2016: https://infectioncontrol.tips/2016/01/14/zika-cases-confirmed-in-north-america-time-to-panic/ […]
[…] articles about having #perspective in regards to the last two public health threats – ebola and zika. Indeed, both are very concerning and scary in many ways. But, did you know that ebola has killed […]